This electronic version has been made freely available under a Creative Commons (CC-BY-NC-ND) license. A copy of the license can be viewed at http://creativecommons.org/licenses/by-nc-nd/2.0/.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
ABSTRACT
Thyroid storm is an acute and life-threatening worsening of hyperthyroidism, characterized by an exacerbation of symptoms and signs of hyperthyroidism, with high fever, dehydration, marked tachycardia or tachyarrhytmias, heart failure, hepatomegaly, respiratory distress, abdominal pain, delirium, possibly seizures. It may occur in patients submitted to thyroidectomy or radioactive iodine treatment while hyperthyroid, or as a consequence of infections in unteated hyperthyroid patients. Treatment consists of antithyroid drug treatmnt, rest, sedation, fluid and electrolyte replacement, cardio-supportive therapy, oxygen therapy, antibiotics, cooling. Mortality is about 10%.
Graves’ orbitopathy (GO) is the main extrathyroidal manifestation of Graves’ disease, found in about 25% of patients at diagnosis, often mild and self-remitting. Removal of risk factors (refrain from smoking, correction of thyroid dysfunction, oral steroid prophylaxis after radioactive iodine therapy, antioxidant therapy with seleniomethionine) are fundamental to prevent progression of mild GO to more severe forms. In moderate-to-severe and active GO, intravenous glucocorticoids are the first-line treatment, second line treatments include cyclosporine, orbital radiotherapy, rituximab (controversial). Novel biologicals, such as teprotumumab and tocilizumab are under investigation. Rehabilitative surgery (orbital decompression, squint surgery, eyelid surgery) is often required. Thyroid dermopathy (pretibial myxedema) is a rare complication of Graves’ disease, usually observed in patients who also have severe GO. Topical glucocorticoids are usually effective. Thyroid acropachy (clubbing of fingers and toes, with swelling of hands and feet) is an extremely rare conditions, for which no treatment is available.
Hypertyroidism may be complicated by severe cardiovascular manifestations, such as tachyarrhythmias (most commonly atrial fibrillation), congestive heart failure, angina, particularly in the elderly or in patients with preexisting heart abnormalities. Prompt restoration of euthyroidism is, therefore, warranted, as well as specific treatments for the heart.
THYROID STORM
Thyroid (or thyrotoxic) storm is an acute, life-threatening syndrome due to an exacerbation of thyrotoxicosis. It is now an infrequent condition, because of earlier diagnosis and treatment of thyrotoxicosis, better pre- and postoperative medical management. However, acute exacerbation of thyrotoxicosis caused by intercurrent illness, especially infections, may still occur. Thyroid storm in the past most frequently occurred after surgery, but now it is usually a complication of untreated or partially treated thyrotoxicosis, rather than a postoperative complication.
Clinical pattern
Classic features of thyroid storm are indicative of a sudden and severe exacerbation of thyrotoxicosis, with fever, marked tachycardia, tremor, nausea and vomiting, diarrhea, dehydration, restlessness, extreme agitation, delirium or coma. Fever is typical and may be higher than 105.8 F (41 C). Patients may present with a true psychosis or a marked deterioration of previously abnormal behavior. Sometimes thyroid storm takes a strikingly different form, called apathetic storm, with extreme weakness, emotional apathy, confusion, absent or low fever
Signs and symptoms of multiple organ failure may be present. Delirium is one example. Congestive heart failure may also occur, with peripheral edema, congestive hepatomegaly, and respiratory distress. Marked sinus tachycardia or tachyarrhythmias, such as atrial fibrillation, are common. Liver damage and jaundice may derive from congestive heart failure or a direct action of thyroid hormone on the liver coupled with malnutrition (Chapter 10). Fever and vomiting may produce dehydration and prerenal azotemia. Abdominal pain may be a prominent feature. The clinical picture may be masked by a secondary infection such as pneumonia, a viral infection, or infection of the upper respiratory tract. Death may be caused by cardiac arrhythmia, congestive heart failure, hyperthermia, or other unidentified factors.
Storm is typically associated with Graves' disease, but it may occur in patients with toxic nodular goiter (1, 2). At present, although still life-threatening, death from thyroid storm is rarer if it is promptly recognized and aggressively treated in an intensive care unit. In recent nationwide studies from Japan mortality rate was >10% (3, 4).
Incidence
In Nelson and Becker's series reported in 1969 (5), there were 21 cases of thyroid storm among 2,329 admissions due to thyrotoxicosis (about 1%). Other series, which included all cases with fever of 38.3 C or more in the postoperative period, reported an incidence of thyroid storm as high as 10% of patients operated on (6). Few patients are now seen with the classic pattern of thyroid storm, but patients are occasionally encountered with marked accentuation of symptoms of thyrotoxicosis in conjunction with infection. The incidence of thyroid storm currently may currently be as low as 0.2 cases/100,000 population (3).
Cause
Thyroid storm classically began a few hours after thyroidectomy performed on a patient prepared for surgery by potassium iodide alone. Many such patients were not euthyroid and would not be considered appropriately prepared for surgery by current standards. Exacerbation of thyrotoxicosis is still seen in patients sent too soon to surgery, but it is unusual in the antithyroid drug-controlled patient. Thyroid storm occasionally occurs in patients operated on for some other illness while severely thyrotoxic. Severe exacerbation of thyrotoxicosis is rarely seen following 131-I therapy for hyperthyroidism; some of these may be defined as thyroid storm (7). Thyroid storm appears most commonly following infection (1), which seems to induce an escape from control of thyrotoxicosis. Pneumonia, upper respiratory tract infection, enteric infections, or any other infection can cause this condition. The decreased incidence of thyroid storm can be largely attributed to improved diagnosis and therapy. In most cases, thyrotoxicosis is recognized early and treated by measures of predictable therapeutic value. Patients are routinely made euthyroid before thyroidectomy or 131-I therapy (8). Using thionamides preoperatively, thyroid glands have only minimal amounts of stored hormones, thus minimizing thyroid hormone release due to manipulation.
Diagnosis
Diagnosis of thyroid storm is made on clinical grounds and involves the usual diagnostic measures for thyrotoxicosis. Semi-quantitative scales and related scores evaluating the presence and severity of clinical manifestations may be of some help in confirming the diagnosis (1, 3, 9). There are no peculiar laboratory abnormalities. Free T4 and, if possible, free T3 should be measured. Serum total T3 may be not particularly elevated or even normal, due to reduced T4 to T3 conversion as observed in nonthyroidal illness (1). Electrolytes, blood urea nitrogen (BUN), blood glucose, liver function tests, and plasma cortisol should be monitored.
Therapy
Thyroid storm is an endocrine emergency that has to be treated in an intensive care unit (Table 12-1).
Table 1. Treatment of Thyroid Storm
Supportive Measures
1. Rest
2. Mild sedation, or anticonvulsant therapy if convulsions occur
3. Fluid and electrolyte replacement
4. Nutritional support and vitamins as needed
5. Oxygen therapy
6. Nonspecific therapy as indicated
7. Antibiotics
8. Cardio-supportive
9. Cooling
Specific therapy
1. Propranolol (20 to 200 mg orally every 6 hours, or 1 to 3 mg intravenously every 4 to 6 hours)
2. Antithyroid drugs (150 to 250 mg PTU or 15 to 25 mg methimazole, every 6 hours)
3. Potassium iodide (one hour after first dose of antithyroid drugs):
4. 100 mg KI every 12 hours
5. Dexamethasone (2 mg every 6 hours)
Possibly useful therapy
1. Ipodate (Oragrafin) or other iodinated contrast agents, if available
2. Plasmapheresis or exchange
3. Oral T4 and T3 binding resins
4. Dialysis
If drugs cannot be given orally (e.g., in the unconscious patient), they can be administered by naso-gastric tube or enemas (1). In some European countries intravenous preparations have been used (10). If the thyrotoxic patient is untreated, an antithyroid drug should be given. PTU, 150-250 mg every 6 hours should be given, if possible, rather than methimazole, since PTU also prevents peripheral conversion of T4 to T3, thus more rapidly reduces circulating T3 levels. Methimazole (15-25 mg every 6 hours) can be given orally, or if necessary, the pure compound can be made up in a 10 mg/ml solution for parenteral administration. Methimazole is also absorbed when given rectally in a suppository. An hour after a thionamide has been given, iodide should be administered. A dosage of 100 mg twice daily is more than sufficient. Unless congestive heart failure contraindicates it, propranolol or other beta-blocking agents should be given at once, orally or parenterally in large doses, depending on the patient's clinical status. Permanent correction of thyrotoxicosis by either 131-I or immediate thyroidectomy should be postponed until euthyroidism is restored. Other supporting measures should fully be exploited, including sedation, oxygen, treatment for tachycardia or congestive heart failure, rehydration, multivitamins, occasionally supportive transfusions, and cooling the patient to lower body temperature down. Antibiotics may be given on the presumption of infection while results of culture are awaited.
The adrenal gland may be limited in its ability to increase steroid production during thyrotoxicosis. If there is any suspicion of hypoadrenalism, hydrocortisone (100-200 mg/day) or its equivalent should be given. The dose can rapidly be reduced when the acute process subsides. Pharmacological doses of glucocorticoids (2 mg dexamethasone every 6 h) acutely depress serum T3 levels by reducing T4 to T3 conversion. This effect of glucocorticoids is beneficial in thyroid storm and supports their routine use in this clinical setting. Propranolol controls tachycardia, restlessness, and other symptoms.
Usually rehydration, repletion of electrolytes, treatment of concomitant disease, such as infection, and specific agents (antithyroid drugs, iodine, propranolol, and corticosteroids) produce a marked improvement within 24 hours. A variety of additional approaches have been reported, but indications for their use are not well defined. For example, oral gallbladder contrast agents such as ipodate and iopanoic acid in doses of 1-2 g, which inhibit peripheral T4 to T3 conversion, might have value. Unfortunately, these agents are no longer available. Peritoneal dialysis can remove circulating thyroid hormone, and plasmapheresis can do likewise, but at the expense of serum protein loss. Orally administered ion-exchange resin (20-30g/day as Colestipol-HCl) can trap hormone in the intestine and prevent recirculation. These treatments are rarely needed.
Antithyroid treatment should be continued until euthyroidism is achieved, when a final decision regarding antithyroid drugs, surgery, or 131-I therapy can be made.
GRAVES’ ORBITOPATHY
Graves’ orbitopathy (GO) is the main and most frequent extrathyroidal manifestation of Graves’ disease, although it may less frequently occur in patients with Hashimoto’s thyroiditis or apparently without thyroid abnormalities (so-called Euthyroid Graves’ disease) (11-15).
Epidemiology

Fig. 1: Prevalence of GO in a series of 346 patients with newly diagnosed Graves’ hyperthyroidism. Moderate-to-severe GO includes one case of sight-threatening dysthyroid optic neuropathy (DON). Derived from Tanda ML et al. (17).
Data on the incidence of GO are limited (11, 14). In a population-based setting in USA, an adjusted rate of 16 cases per 100.000 per year in women and 2.9 cases per 100.000 in men was reported (16). In a recent study of a large cohort of newly diagnosed Graves’ patients, about 75% had no ocular involvement at diagnosis, only 6% had moderate-to-severe GO, and 0.3% showed sight-threatening GO due to dysthyroid optic neuropathy (DON) (17) (Figure 1). In a Danish population, moderate-to-severe GO showed an incidence of 16.1/million per year (women: 26.7; men: 5.4) (18). Ocular involvement is in most cases bilateral, although often asymmetrical, but it may be unilateral in up to 15% of cases (12, 14). As recently reviewed by the European Group on Graves’ Orbitopathy (EUGOGO), the overall prevalence of GO in Europe is about 10/10,000 patients, but the prevalence of its variants (hypothyroid GO, GO associated with dermopathy, GO associated with acropachy, asymmetrical or unilateral GO) is much lower, and recently euthyroid GO has been listed as a rare disease in Europe (19). The onset of GO apparently has a bimodal peak in the fifth and seventh decades of life, but eye disease may occur at any age (20). It is more frequent in women, but men tend to have a more severe disease (21-23), as suggested by a decrease in the female/male ratio from 9.3 in mild GO, to 3.2 in moderately severe GO, and 1.4 in severe GO (20). There is a close temporal relationship between the onset of GO and the onset of hyperthyroidism. In approximately 85% of cases GO and hyperthyroidism occur within 18 months of each other (20), although GO may both precede (about 20% of cases) or follow (about 40% of cases) the onset of hyperthyroidism (20).
The natural history of GO is poorly understood. However, in a longitudinal cohort study, spontaneous amelioration was observed in two thirds of cases, while ocular involvement did not change with time in 20% and progressed in 14% (22). The observation that mild GO rarely progresses and often spontaneously remits was recently confirmed by a large prospective study of patients with recent onset Graves’ hyperthyroidism (17) and summarized in a review of published studies (24). It is worth noting that GO seems to be less frequent than in the past. A review of the first 100 consecutive patients seen at the same joint thyroid-eye unit in 1960 and 1990 revealed a decrease in the proportion of Graves’ patients with clinical relevant GO from 57% to 32% (23); likewise, a reduction in the proportion of severe forms of GO compared to milder forms was observed (18), likely reflecting an earlier diagnosis and treatment of both hyperthyroidism and orbitopathy. It should be noted that a multicenter study carried out by the European Group on Graves’ Orbitopathy (EUGOGO) reported that 40% of GO patients had mild disease, 33% had moderate GO, and 28% had severe eye disease (25). It should be noted that these figures were clearly influenced by the fact that EUGOGO centers are all referral centers where it is likely to see more complicated cases of GO. Accordingly, a recent single-center study confirmed that most patients newly diagnosed with Graves’ disease have mild GO (26), although whether these forms are chronic remitting or a transient disease (27) or whether GO ever disappears completely (28) is unsettled. In summary, based on recent studies and reviews of the available literature, it can be concluded that GO is a rare disease, particularly in its severe expressions (19).
An important epidemiologic feature of GO is its relation with cigarette smoking (29,30). The prevalence of smokers among Graves’ women with orbitopathy is much higher than that in Graves’ women apparently without GO or in normal controls (Figure 2) (31). Smoking is a predictor of Graves’ hyperthyroidism, with a hazard ratio of 1.93 in current smokers, 1.27 in ex-smokers, and 2.65 in heavy smokers (32). In a case-control study, the odds ratio of cigarette smoking for Graves’ hyperthyroidism without GO was 1.7, but raised to 7.7 for Graves’ disease with GO (33). Whether passive smoking may have the same impact as active smoking is unsettled; however, in a recent European survey of GO in childhood, the highest prevalence of Graves’ children with GO was found in countries where the prevalence of smokers among teenagers was also highest: since >50% of children were <10 years of age, it is likely that passive smoking rather than active smoking influenced GO occurrence (34). Mechanisms whereby smoking may affect the development and course of GO are unclear. In addition to direct irritative effects and modulation of immune reactions in the orbit (35), smoking was associated with an increase in the orbital connective tissue volume as assessed by MRI (36), and with an increased adipogenesis and hyaluronic acid production in in vitro cultured orbital fibroblasts (37). Whatever the mechanism(s) involved, cigarette smoking is strong (probably the strongest) predictor of GO occurrence in patients with Graves’ hyperthyroidism (38).
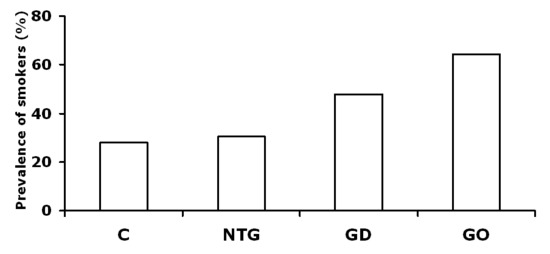
Figure 2. Prevalence of smokers among women with Graves’ disease with (GO) or without (GD) associated orbitopathy. NTG: Non-toxic goiter; C: controls. Derived from Bartalena et al (31).
Pathogenesis
Clinical manifestations of GO reflect remodeling of the orbital space related to the enhanced orbital volume, due to an increase in retroocular fibroadipose tissue and swelling of extraocular muscles (39-41). Orbital tissues, including muscles, are infiltrated by inflammatory cells, including lymphocytes, mast cells, and macrophages. Proliferation of orbital fibroblasts and adipocytes, both in the retroocular space and in the perimysial space, is also associated with an increased production of glycosaminoglycans, which are the ultimate responsible for edematous changes both in the connective tissue and the muscles, owing to their hydrophilic nature. The relative contribution of the increase in fibroadipose tissue volume and extraocular muscle swelling is not always the same, and a predominance of either component may be observed in different patients with similar clinical features (42). Furthermore, the increase in orbital fat might be a rather late phenomenon (43). Because the orbit is a rigid, bony structure anteriorly limited by the orbital septum, the increased orbital volume deriving from cell proliferation, inflammatory infiltration and edema, results into enhanced intraorbital pressure, forward displacement of the globe (proptosis or exophthalmos), extraocular muscle dysfunction causing diplopia and/or strabismus, soft tissue changes with periorbital edema, conjunctival hyperemia and chemosis. If proptosis, which can be considered a form of spontaneous decompression, is severe, subluxation of the eye may occur. Proptosis is responsible for corneal exposure which may be particularly dangerous at night for the incomplete eyelid closure (lagophthalmos), and may result into sight-threatening corneal ulceration. The enlarged muscle volume may cause optic nerve compression (dysthyroid optic neuropathy), especially if the orbital septum is tight and proptosis is minimal. Optic nerve compression is particularly evident at the orbital apex and may be responsible for sight loss. Orbital inflammation and related anatomical changes may cause venous and lymphatic congestion that contribute to periorbital edema and chemosis. With time inflammation subsides and muscle fatty degeneration and fibrosis may contribute to further extraocular muscle restriction and strabismus, which, at this stage, can only be corrected by surgery.
GO is an autoimmune inflammatory disorder related to the thyroid and triggered by the migration of autoreactive T-helper cells into the orbit, which is infiltrated by CD4+ T cells and, to a lesser extent, CD8+ T cells, B cells, fibrocytes, mast cells, and macrophages (40, 41). Orbital fibroblasts are the main target and key effector cells in the disease (44). After recognition of one or more antigens (shared with the thyroid) on fibroblast surface, facilitated by HLA class II antigen expression on antigen-presenting cells (B cells, macrophages), CD4+ T cells secrete cytokines which activate CD8+ T cells, autoantibody-synthesizing B cells (45) and stimulate orbital fibroblasts (46). Fibroblasts proliferate, may differentiate into myofibroblasts and adipocytes, accumulate and secrete hyaluronic acid (HA), synthesize and secrete chemoattractants (interleukin-16, RANTES, CXCL10) and a number of cytokines (interleukin-1, interleukin-6, interferon-g, tumor necrosis factor-a, interleukin-8, interleukin-10, platelet-derived growth factor, transforming growth factor-b), which concur to auto-maintain the inflammatory process (47). HA is hydrophilic and thereby attracts water and causes edema of the extraocular muscles and orbital tissue (40). Orbital fibroblasts can be differentiated based on the expression or lack of expression of a cell surface glycoprotein (thymocyte antigen-1, thy-1). Thy-1+ fibroblasts are mostly represented in extraocular muscles and produce HA, thereby contributing to extraocular muscle edema and enlargement, whereas thy-1- fibroblasts are mainly present in connective tissue and may differentiate into adipocytes, thereby contributing to fibroadipose tissue expansion (40).
The TSH receptor (TSH-R), the ultimate cause of hyperthyroidism due to Graves’ disease, is likely the shared antigen responsible for GO. TSH-R expression has been shown in the orbital tissue of GO patients, both at the mRNA and protein levels (48, 49); however, TSH-R is also expressed in several other tissues not involved in Graves’ disease and orbitopathy (50), and, although at lower levels, in normal orbital fibroadipose tissue samples and cultures (51). On the other hand, BALB/c mice injected with spleen cells primed either with a TSH-R fusion protein or with TSH-R cDNA developed thyroiditis with blocking-type TRAb, but also showed orbital pathological changes (lymphocytic and mast cell infiltration, edema, presence of glycosaminoglycans) similar to those seen in human GO (52). This model could not be reproduced in other laboratories. More recently a novel preclinical female mouse model of GO was established (53). In this model, some of the mice immunized by human TSH A-subunit by TSH receptor plasmid in vivo electroporation showed large infiltrates surrounding the optic nerve, increased adipogenesis, orbital muscle hypertrophy, exophtahlmos, and chemosis (53, 54). The role of the TSH-R seems to be supported also by other animal models (55-57). Another putative antigen involved in the pathogenesis of GO is the IGF-1 receptor. As recently reviewed (58), increased IGF-1 receptor levels have been reported in orbital fibroblasts as well as in B and T lymphocytes from Graves’ patients, and immunoglobulins displacing IGF-1 from its binding to the IGF-1 receptor have also been found in these patients (59). Colocalization of TSH receptor and IGF-1 receptor has been shown both in orbital fibroblasts and thyrocytes, suggesting that the two receptors might form a functional complex (60). Stimulation of the TSHR by the monoclonal TSHR-stimulating antibody, M22, could be inhibited by an IGF-1R-blocking monoclonal antibody in orbital fibroblasts (61). Involvement of the IGF-1R is not specific for Graves’ disease, since it is implicated in other autoimmune diseases, such as rheumatoid arthritis (62). Thus, although involvement of the IGF-1R in the pathogenesis of GO seems likely (63), it is tempting to speculate, for the time being, that autoimmunity to the TSH receptor be the initiating mechanism, while subsequent increased expression of the IGF-1R might be fundamental to maintain ongoing reactions in the orbit (64). Interestingly, two recent reports found that, at variance with TRAb, only a minority of patients with GO have circulating antibodies to the IGF-1R (65, 66). This may be related to the low sensitivity and specificity of tests used to detect such antibodies (62). Alternatively, it may be conceived that IGF-1 (and/or IGF-1R antibodies) locally produced in the orbit be relevant for the pathogenesis of GO (67).
Other autoantigens, including several eye muscle antigens, acetylcholine receptor, thyroperoxidase, thyroglobulin, alpha-fodrin, have been proposed as putative shared antigens, but their true role is, to say the least, uncertain (68).
The role of genetic factors in the pathogenesis of GO is not very well defined, and no striking differences have been observed between Graves’ patients with or without associated GO (69-73). An association between GO and Major Histocompatibility Complex (MHC), cytotoxic T-lymphocyte-associated antigen-4 (CTLA-4) or intercellular adhesion molecule 1 gene polymorphisms has been looked for, but results are not unequivocal (74-76). GO likely stems from a complex interplay between endogenous factors and exogenous (environmental) risk factors (13, 77). The latter are probably more important and include cigarette smoking, thyroid dysfunction, and, in a subset of patients, radioiodine therapy for Graves’ hyperthyroidism (13, 77). The relationship between cigarette smoking and GO has been discussed above (see paragraph on Epidemiology). Both hyperthyroidism (78, 79) and hypothyroidism (80) seem to influence negatively the course of the orbitopathy. TRAb are independent risk factors for GO and can help to predict severity and outcome of eye disease (81). Radioiodine therapy for Graves’ hyperthyroidism is associated with GO progression in about 15% of cases, although this effect may be transient (82-86). This effect is more frequently observed in patients who already have GO prior to radioiodine therapy, smoke, have high TRAb levels, or whose post-radioiodine hypothyroidism is not promptly corrected by L-thyroxine replacement therapy (13, 77). Radioiodine-associated progression of GO can be prevented by a short course of prednisone (87). Lower doses of oral prednisone (0.2 mg/Kg bw) for 6 weeks are as effective in preventing RAI-associated progression of GO as higher doses used in the past (88). Neither thyroidectomy (typically partial) nor antithyroid drugs influence the course of the orbitopathy (89-91). The above observations have important practical implications in terms of GO prevention (Table 2), because GO patients should be urged to refrain from smoking, their thyroid dysfunction (both hyper- and hypothyroidism) should be promptly corrected, and, in the case of radioiodine therapy, a short course of oral prednisone should be administered (92).
Table 2. Risk factors for the occurrence/progression of Graves’ orbitopathy and preventive measures
|
Risk factor |
Preventive measure |
Cigarette smoking | Refrain from smoking |
Hyperthyroidism | Restore euthyroidism by antithyroid drugs and/or obtain a permanent control by thyroid ablation (thyroidectomy, radioiodine, both) |
Hypothyroidism | Restore euthyroidism by L-thyroxine replacement therapy |
Radioiodine therapy for hyperthyroidism | Give oral prednisone concomitantly with radioiodine administration. Avoid leaving the patient with untreated post-radioiodine hypothyroidism |
High TSH-receptor antibody levels | Control hyperthyroidism as soon as possible |
| Oxidative stress | Give a 6-month selenium course in mild GO |
Clinical Features
Signs & Symptoms. Clinical features of GO include soft tissue changes, exophthalmos, extraocular muscle dysfunction, corneal abnormalities, and optic nerve involvement (Figures 3-6). The NOSPECS classification (Table 3) is a useful memory aid of GO abnormalities (93). Recommendations for GO assessment in clinical practice have recently been reviewed by EUGOGO (94) and other groups (VISA classification) (95). Soft tissue changes include eyelid edema and periorbital swelling, eyelid erythema, conjunctival hyperemia and chemosis, inflammation of the caruncle or plica: their assessment and grading can be done with the aid of a color atlas (96), which can be downloaded from EUGOGO website (www.eugogo.eu). Proptosis, i.e., protrusion of the eye (exophthalmos), is usually measured by Hertel exophthalmometer; normal values are usually less than 20 mm, but vary with race, age, gender, degree of myopia, and should be established in each center or institution. Extraocular muscle dysfunction is responsible for diplopia (double vision), which can be subjectively defined as intermittent (i.e., present only when fatigued or when first waking), inconstant (i.e., present only at extremes of gaze), or constant (i.e., present also in reading positions and primary gaze); objective assessment of extraocular muscle functioning can be done by several methods, including measurement of duction in degrees (94). Palpebral aperture may be increased due to several factors, including upper and/or lower lid retraction, and proptosis. Lid retraction and proptosis are responsible for corneal exposure, which may lead to corneal epithelium damage (punctate keratopathy), corneal ulceration and perforation. The incomplete eye closure at night (lagophthalmos) and the absence of Bell’s phenomenon (no upward eye rotation on attempted eye closure) are risk factors for corneal damage (92, 94). Intraocular pressure is often increased, particularly in upward gaze, but this abnormality rarely progresses to true glaucoma. Dysthyroid optic neuropathy, due to optic nerve compression at the orbit apex by swollen extraocular muscles, or, less frequently, to optic nerve stretching in cases of marked proptosis or eye subluxation, is a sight-threatening expression of GO. It can be diagnosed by fundoscopy showing disc swelling, reduced visual acuity, abnormal color vision test, contrast sensitivity, perimetry, visual-evoked potentials, and pupillary responses (95).

Figure 3. Female patient with moderately severe GO. Note periorbital swelling, injection of conjunctival vessels, proptosis, marked lid retraction, and proptosis.

Figure 4. Male patient with moderately severe GO. Note marked periorbital swelling, conjunctival hyperemia, esotropia (strabismus) in the left eye.

Figure 5. Male patient with moderately severe GO. Note the superior eyelid edema, mild conjunctival vessel injection, marked proptosis, and marked upper lid retraction.

Figure 6. Female patient with severe GO. Note marked periorbital swelling, palpebral hyperemia, conjunctival hyperemia, proptosis (particularly in the left eye), caruncle edema. Eye motility was markedly reduced, lagophthalmos was present, there were two corneal ulcers in the left eye, and corneal punctate staining in the right eye, reduced visual acuity in the left eye (5/10). CT scan showed enlargement of extraocular muscles (particularly medial rectus and inferior rectus) in both eyes, but no relevant compression of the optic nerve at the orbit apex.
Table 3. NOSPECS classification of eye changes of Graves’ disease
|
Class |
Grade |
Symptoms and Signs |
0 | No symptoms or signs | |
1 | Only signs (upper lid retraction, without lid lag or proptosis) | |
2 | Soft tissue involvement with symptoms (excess lacrimation, sandy sensation, retrobulbar discomfort, and photophobia, but not diplopia);objective signs as follows: | |
0 | absent | |
a | minimal (edema of conjunctivae and lids, conjunctival injection, and fullness of lids, often with orbital fat extrusion, palpable lacrimal glands, or swollen extraocular muscles beneath lower lids) | |
b | Moderate (above plus chemosis, lagophthalmos lid fullness) | |
c | marked | |
3 | Proptosis associated with classes 2 to 6 only (specify if inequality of 3 mm or more between eyes, or if progression of 3 mm or more under observation) | |
0 | absent (20 mm or less) | |
a | minimal (21-23 mm) | |
b | moderate (24-27 mm) | |
c | marked (28 mm or more) | |
4 | Extraocular muscle involvement (usually with diplopia) | |
0 | absent | |
a | minimal (limitation of motion, evident at extremes of gaze in one or more directions) | |
b | moderate (evident restriction of motion without fixation of position) | |
c | marked (fixation of position of a globe or globes) | |
5 | Corneal involvement (primarily due to lagophthalmos) | |
0 | absent | |
a | minimal (stippling of cornea) | |
b | moderate (ulceration) | |
c | marked (clouding, necrosis, perforation) | |
6 | Sight loss (due to optic nerve involvement) | |
0 | absent | |
a | minimal (disc pallor or choking, or visual field defect, vision 20/20 to 20/60) | |
b | moderate (disc pallor or choking, or visual field defect, vision 20/70 to 20/200) | |
c | marked (blindness, i.e., failure to perceive light; vision less than 20/200) | |
From Werner (93). | ||
Symptoms of GO (Table 4) include, in addition to changes in ocular appearance related to periorbital swelling and proptosis, excess lacrimation, photophobia, grittiness, pain in or behind the eyes, either spontaneous or with eye movements, diplopia of different severity with or without strabismus, blurred vision, which may clear with blinking (due to excessive lacrimation) or covering one eye (reflecting extraocular muscle impairment), or may persist (probably reflecting optic neuropathy, particularly if associated with gray areas in the field of vision). In addition to reduced visual acuity, optic nerve involvement can be heralded by decreased color perception. Diplopia may be absent if extraocular muscle involvement is symmetrical in both eyes.
Table 4. Symptoms associated with Graves’ orbitopathy
1. Changes in eye appearance, particularly eyelid or periorbital swelling, eye bulging
2. Excessive lacrimation, often more pronounced on waking
3. Incomplete closure of eyes at night (lagophthalmos), as reported by the partner
4. Photophobia, need to protect eyes with dark lenses
5. Increased eye “sensitivity” to irritative factors other than light (e.g., wind, smoke, pollution)
6. Ocular discomfort, described as grittiness, foreign body or sandy sensation, often defined as “allergy”
7. Ocular pain, either related or unrelated to eye movements
8. Neck ache, with abnormal head posture (torcicullum)
9. Diplopia
a. Intermittent: present only when tired or on waking
b. Inconstant: present only at extremes of gaze
c. Constant: present also in primary and reading positions
10. Blurred vision
a. Disappearing with blinking
b. Not disappearing with blinking
11. Reduced color perception
Clinical manifestations of GO have a profound negative impact on quality of life and daily activities of affected individuals (98). By the use of general health-related quality of life (HRQL) questionnaires, such as the SF-36 or its shorter forms, it was shown that GO is associated with significant changes in several functions, including physical functioning, role functioning, social functioning, mental health, general health perception, and bodily pain (99). Interestingly, these changes in HRQL parameters were similar to those found in patients with inflammatory bowel disorders, and even more marked than those observed in patients with diabetes mellitus, heart failure or emphysema (99). Since HRQL questionnaires are broad and may not address items specific for a given disease, a GO-specific quality of life (GO-QoL) questionnaire was developed and validated in clinical studies (99, 100-102). This questionnaire (dowloadable from EUGOGO website at www.eugogo.eu) is composed of 16 questions, 8 concerning the consequences of diplopia and deceased visual acuity on visual functioning, and 8 regarding the consequences of changes in physical appearance on social functioning. The Go-QoL is a useful tool for self-assessment of treatment outcomes for GO (103).
Activity & Severity. Definition of GO severity is somehow arbitrary and may reflect different views (11, 23). According to the most recent EUGOGO definition (92), mild GO is characterized by one or more of the following features: minor lid retraction (<2 mm), mild soft tissue involvement, exophthalmos <3 mm above normal for race and gender, transient or no diplopia, and corneal exposure; the above features usually have a minor impact on daily life to justify immmuno-suppression or surgical treatment; moderate-to-severe GO have any one or more of the following: lid retraction >2 mm, moderate or severe soft tissue involvement, exophthalmos >3 mm above normal for race and gender, inconstant or constant diplopia; Patients in this category have an impact on daily life as to justify immunosuppression (if GO is active) or surgical intervention (if GO is inactive); sight-threatening GO is due to dysthyroid optic neuropathy (DON) or corneal breakdown, and warrants immediate intervention (Table 5) (92). Assessment of severity is particularly relevant to decide on whether a given patient should be treated by aggressive treatments (either medical or surgical) or simply by local or general supportive measures (see below).The other important feature of GO is its activity. Although, as stated above, GO natural history is not completely understood, it is commonly accepted that GO undergoes an initial phase of activity, characterized by progressive exacerbation of ocular manifestations until a plateau phase is reached; GO then tends to remit spontaneously, but remission is invariably partial. In the inactive phase (burnt-out GO), only residual ocular manifestations are present (e.g., proptosis, strabismus due to muscle fibrotic changes), but inflammation has subsided and it is unlikely that it may flare up. It is unknown how long this process takes to be completed, but it is widely believed that it takes between 6 months and two years. Recognition of the different phases of the disease is important, because active disease, basically characterized by the presence of inflammation, can respond to immunosuppressive treatments, which are largely ineffective when GO is burnt-out. Different indicators have been proposed to assess GO activity, including short duration of treatment (<18 months), positivity of octreoscan, decreased extraocular muscle reflectivity at orbital ultrasound, prolonged T2 relaxation time at MRI, increased urinary glycosaminoglycan levels, but they lack sufficient specificity and accuracy. A useful tool to assess GO activity is represented by the Clinical Activity Score (CAS), which can be calculated very easily and is recommended by EUGOGO in the assessment of GO in routine clinical practice, in specialist multidisciplinary clinics, and for clinical trials (92). In its original formulation (104) it included 10 items, which were subsequently reduced to 7 when revised by an ad hoc Committee of the four sister thyroid societies (105). (Table 6). If one point is given to each item when present, CAS, which basically reflect eye inflammation, may range from 0 (absent activity) to 7 (maximal activity); GO is generally defined active if CAS is >3.
Table 5. Assessment of severity of Graves’ orbitopathy
| Degree of Ocular involvement | Features |
| Mild GO | Minor lid retraction (<2 mm), mild soft tissue involvement, exophthalmos <3 mm
above normal for race and gender, transient or no diplopia, corneal exposure responsive to lubricants |
| Moderate-to-severe GO | Lid retraction >2 mm, moderate-to-severe soft tissue involvement, exophthalmos >3 mm
above normal for race and gender, inconstant or constant diplopia |
| Sight-threatening GO | Presence of dysthyroid optic neuropathy and/or corneal breakdown |
Derived from Bartalena & EUGOGO (92)
Table 6. Clinical Activity Score (CAS).
| 1. Spontaneous retrobulbar pain
2. Pain on eye movements 3. Eyelid erythema 4. Conjunctival injection 5. Chemosis 6. Swelling of the caruncle 7. Eyelid edema or fullness |
One point is given to each item, if present. CAS is the sum of single scores, ranging from 0 (no activity) to 7 (maximal activity). Active GO: CAS>3 |
From Mourits et al (104), modified from an ad hoc Committee of the four Thyroid sister Societies (105). |
Diagnosis
Diagnosis of GO is usually easy on clinical grounds and by careful ophthalmological examination. Although not necessary in most Graves’ patients, CT scan or MRI of the orbit confirm diagnosis by showing enlarged extraocular muscles (without involvement of the tendon) and/or increased orbital fibroadipose tissue (106). Modest extraocular muscle enlargement and increased fibroadipose tissue volume are often found in Graves’ patients without clinical manifestations of ocular involvement. Orbital imaging is very useful to detect signs of optic nerve compression, which support the diagnosis of optic neuropathy. Imaging is required in asymmetrical or, particularly, unilateral forms of GO, to rule out that proptosis, periorbital swelling, inflammation, or diplopia be due to disorders other than GO (12, 106). The latter include primary or metastatic orbital tumors, vascular abnormalities (e.g., carotid-cavernous sinus fistula, carotid aneurysm, cavernous sinus thrombosis, subarachnoid hemorrhage, subdural hematoma), granulomatous disorders, IgG4-related ophthalmic disease (107). Occasionally, angiograms or venograms may be required for diagnosis. Octreoscan may be useful to identify patients with active GO (106), but its role in clinical practice is limited, also in view of its high cost.
Management
Management of GO is based on a multidisciplinary approach which involves endocrinologists, ophthalmologists, orbit surgeons, radiologists and radiotherapists. In a survey of GO management based on a questionnaire distributed among members of the European Thyroid Association, European Society of Ophthalmic Plastic and Reconstructive Surgery, and European Association of Nuclear Medicine, 96% of responders stated that a multidisciplinary setting for GO management is valuable, although 21% of patients were in the end not treated in a multidisciplinary setting (108). The therapeutic approach to a GO patient should be based on both severity and activity of the disease, the former being the feature to assess first.
Mild GO. Most patients have mild GO, which does not require particularly aggressive treatments and often is self-limiting (92, 110, 111). If GO activity is modest, simple local measured can be suggested to obtain symptomatic relief until GO is burnt-out (Table 7). Photophobia can be mitigated by sunglasses; grittiness due to corneal exposure can be controlled by artificial tears and topical lubricants, particularly indicated in the presence of lagophthalmos; the latter may require taping the eyelids shut at night; eyelid retraction can be controlled (with a variable degree of success) by b-blocking drops (useful for the increased intraocular pressure) or by botulinum toxin injections (112); elevation of the bed may be helpful to reduce periorbital swelling due to congestion; mild diplopia often is controlled by prisms (if they are tolerated). Reassurance is an important issue, and the patient must be informed that his/her eye disease is unlikely to progress to more severe forms, usually stabilizes, and often ameliorates spontaneously. Control of thyroid dysfunction is fundamental, because progression often is associated with hyper- or hypothyroidism (12, 92); refrain from smoking is also essential, because it is associated with a decreased chance of developing proptosis and diplopia (113), and decreases the likelihood to develop severe GO (29). Patients who do not succeed to quit smoking by themselves, should be helped by professional stop-smoking clinics, organizations, groups, where they can receive counseling, behavioral therapies, pharmacological treatments. In a subset of patients with mild GO, the impact of GO on the quality of life is so pronounced as to justify the risk of immunosuppression (or surgery) as for moderate-to-severe GO (92). A recent randomized controlled trial performed by EUGOGO in a large cohort of patients with mild GO showed that selenium supplementation for 6 months has beneficial effects on mild GO compared with placebo and can often prevent its progression to more severe forms (114). Thus, selenium, for its anti-inflammatory and immunomodulatory actions, should be considered both as a therapeutic tool for mild GO and a preventive measure (115). Whether selenium is also useful as an adjuvant therapy in patients with moderate-to-severe GO is presently unsettled.
Table 7. Management of mild Graves’ orbitopathy
|
Sign and/or symptom and/or associated problem |
Therapeutic measure |
Photophobia | Sunglasses |
Foreign body or sandy sensation | Artificial tears and ointments |
Eyelid retraction | alpha-blocking eye drops. Botulinum toxin injections |
Increased intraocular pressure | alpha-blocking eye drops |
Lagophthalmos | Nocturnal eye taping |
Thyroid dysfunction (hyper/hypo) | Restoration of euthyroidism, as appropriate |
Smoking | Refrain from smoking |
Anxiety about possible further progression | Reassurance on the natural history of mild GO |
| Management of clinical picture and prevention of progression | Selenium supplementation |
Moderate-to-severe GO. Management of moderate-to-severe GO depends not only on severity, but also on activity of the orbitopathy (Table 8). Medical treatment is likely to be beneficial in patients with active GO, with florid signs and symptoms of inflammation, recent-onset extraocular muscle dysfunction, recent progression of the ocular abnormalities as a whole. On the contrary, in long-standing GO, with chronic proptosis and residual, stable diplopia and/or strabismus, but no no evidence of inflammation, medical treatment has little chances to produce favorable effects, and the surgical, rehabilitative approach is preferable (92). Dysthyroid optic neuropathy, the most severe expression of the orbitopathy, is a clinical, sight-threatening emergency, which requires immediate treatment. If there is no response to medical treatment (high-dose intravenous glucocorticoids), orbital decompression is warranted (92).
Table 8. Management of moderate-to-severe Graves’ orbitopathy
| Treatment | Validity |
| Glucocorticoids | Established |
| Orbital Radiotherapy | Established |
| Orbital Decompression | Established |
| Rehabilitative Surgery (squint surgery, eyelid surgery) | Established |
| Somatostatin analogs | Non-validated (octreotide, lanreotide) |
| Intravenous immunoglobulins | Non-validated |
| Cyclosporine | Limited applications |
| Antioxidants | Selenium (validated only for mild GO) |
| Rituximab | Two conflicting and small randomized clinical trials |
| Etanercept | Limited data (non-validated in randomized clinical trials) |
| Mycophenolate | Two randomized clinical trials with positive results |
| Teprotumumab | One randomized clinical trial with positive results |
| Thyroid ablation by 131-I and/or surgery | Controversial |
Glucocorticoids are the mainstay in the medical treatment of GO (12, 92, 116, 117). They have been used for decades because of their anti-inflammatory effects, but also because they exert immunosuppressive actions useful to control the course of the orbitopathy (12, 92, 116, 117). The latter include interference with the function of T and B lymphocytes, decreased recruitment of neutrophils and macrophages, down-regulation of adhesion molecules, inhibition of cytokine secretion, inhibition of glycosaminoglycan secretion. Locally (subconjunctivally or retrobulbarly) given glucocorticoids are less effective than systemically given glucocorticoids ) (11, 92), although favorable responses in terms of improvement of diplopia and reduction in extraocular muscle dysfunction have been reported with in a recent randomized clinical trial of periocular injections of triamcinolone acetate (118) . Glucocorticoids have for a long time been given mostly orally. This route of administration has several drawbacks: high doses are required every day (e.g., prednisone 60-100 mg daily as a starting dose, or equivalent doses of other steroids) (11), treatment lasts for several months (at least 5-6 months), recurrences are frequent upon drug tapering or withdrawal, side effects (particularly Cushing’s syndrome) are frequent (12, 92, 116, 117). In the last 20 years the intravenous route has become the most commonly used (101) and currently represents the first-line treatment for moderate-to-severe and active GO (92). Intravenous glucocorticoids are more effective, with a rate of favorable responses reported until few years ago of about 80-90% versus 60-65% with oral glucocorticoids (117, 119), and better tolerated than oral glucocorticoids (120). As a proof of principle, in a placebo-controlled, randomized trial, intravenous methylprednisolone (four cycles at a dose of 500 mg for 3 consecutive days at 4-week intervals) effected inflammatory changes and extraocular muscle dysfunction in 5 of 6 patients (83%) compared to only one of 11 placebo-treated patients (121) Glucocorticoids are most effective on soft tissue, inflammatory changes, recent-onset extraocular muscle dysfunction, and dysthyroid optic neuropathy, whereas proptosis and long-lasting eye muscle impairment are less responsive (11, 117). However, it should be noted that severe liver damage, heralded by a marked rise in serum concentrations of hepatic enzymes, was noted in 7 of about 800 treated patients (approximately 0.8%), three of whom died (122). The causes of this hepatotoxicity are unclear, but might include direct liver toxicity of glucocorticoids, precipitation of virus-induced hepatitis, sudden reactivation of the immune system upon drug withdrawal leading to autoimmune hepatitis. Statins are not a risk factor for liver damage associated with intravenous glucocorticoid pulse therapy for GO (123). The cumulative dose of glucocorticoids might also be important, since no cases of liver damage were reported in a recent randomized clinical trial in which lower, but equally highly effective, doses of glucocorticoids were employed (124). In this trial, the cumulative dose of methylprednisolone was 4.5 grams, subdivided in 12 weekly 2-hour infusions (500 mg for the first 6 infusions, 250 mg for the remaining 6 infusions) (124). A questionnaire-based surgery carried out among members of the European Thyroid Association showed a wide heterogeneity in the regimens of intravenous glucocorticoid therapy for moderate-to severe and active GO (125). A recent mullticenter, randomized clinical trial of a large cohort of patients with moderate-to-severe and active GO showed that a cumulative dose of about 7.5 g of methylprednisolone was associated with more favorable treatment outcomes than lower doses (about 5 g or 2.25 g), but also caused adverse events more frequently (126). Thus, the cumulative dose should somehow be tailored to the severity and activity of GO, reserving the highest dose to patients with most severe expressions of the disease. In any case, the current recommendation is that the cumulative dose of glucocorticoids per course should not exceed 8 grams (92). Response to intravenous glucocorticoids may occur early in the course of the intravenous course, but also later; accordingly, the lack of response after the first 5-6 infusions is not an indication to stop the treatment (127). Adverse events of high-dose glucocorticoid treatment remain a relevant issue (128). Accordingly, patients should be treated in specialized centers under strict medical surveillance (92). Intravenous glucocorticoid treatment of Graves’ ophthalmopathy is not associated with secondary adrenocortical insufficiency. (129, 130),presumably because it is given for a limited period and intermittently.
Orbital radiotherapy is the other non-surgical mainstay in the management of GO (131). The rationale for its use and the indications are quite similar to those of glucocorticoids; in addition, irradiation exploits the radiosensitivity of T lymphocytes which infiltrate the orbit (131). Irradiation is currently carried out by linear accelerators, using a cumulative dose of 20 Gray fractionated in 10 daily 2-Gray doses over a 2-week period (131), although other regimens (and lower doses) might be equally effective (132). Favorable responses have been reported in about 60% of treated patients (131). Recent years have witnessed a lively debate on the true effectiveness of orbital radiotherapy (133, 134). However, the results of several randomized studies confirmed, with one exception, its efficacy (132, 135-138). In addition, orbital radiotherapy is a safe procedure devoid of relevant short-term and long-term side effects or complications (139, 140). Preexisting retinopathy associated with diabetes mellitus or hypertension represents a contraindication to its use (92). As for glucocorticoids, orbital radiotherapy is mostly effective on soft tissue inflammatory changes and recent-onset extraocular muscle dysfunction (131). Orbital radiotherapy can be used either alone or in combination with glucocorticoids. The association exploits the prompter effect of glucocorticoids and the more sustained action of irradiation; in two randomized prospective studies, combined therapy (using oral glucocorticoids) proved to be more effective than either treatment alone (141, 142). Whether the combination of intravenous glucocorticoids and orbital radiotherapy is more effective than intravenous glucocorticoids alone is presently unsettled. For this reason the recent guidelines for the management of moderate-to-severe and active suggest the combination of orbital radiotherapy and oral glucocorticoids as a second-line treatment in the case of a partial or absent response to intravenous glucocorticoids (92).
Cyclosporine, used in GO for its immunosuppressive properties, has been reported in only two randomized and controlled studies (143, 144) . Cyclosporine has a lower efficacy than glucocorticoids as a single-agent therapy, although a combination of both drugs might be more effective than either treatment alone (143, 144). Thus, the use of cyclosporine might be maintained in patients who are relatively resistant to glucocorticoids in whom persistent GO activity warrants continuing medical intervention (145). Side effects of cyclosporine are not negligible and should be carefully considered. As for orbital radiotherapy, no studies have compared the combination of cyclosporine and intravenous glucocorticoids. Therefore, the association of oral glucocorticoids and cyclosporine is considered an alternative option when the response to intravenous glucocorticoids is poor (92).
Rituximab is a CD20+ B-cell depleting monoclonal antibody originally used for B-cell non-Hodgkin lymphoma, but then utilized for autoimmune B-cell (and T-cell) driven autoimmune disorders. This drug has been used for GO in small and uncontrolled preliminary studies (reviewed in refs. 146 and 147). The rationale for using rituximab is sound, based on our understanding of pathogenesis of GO. The available data suggest that rituximab may have favorable effects on moderate-to-severe and active GO, with relatively low adverse event rate (146, 147). Two small, single-center, randomized clinical trials have recently been published. They produced conflicting results, because the first one (148) showed no difference in the effect of rituximab compared to placebo (148), whereas the second one (149) showed that rituximab was as effective as intravenous glucocorticoids in inactivating GO and was not associated with a flare-up of the disease, not infrequently seen after withdrawal of glucocorticoids. The reason for this conflicting results remains elusive and larger multicenter studies are warranted to clarify this issue (150), nevertheless rituximab may be considered as a possible second-line treatment in the case of a partial or absent response to intravenous glucocorticoids (92). Rituximab is contraindicated in patients with overt or impending dysthyroid optic neuropathy (92).
Two recent randomized clinical trials have evaluated the effect of mycophenolate, an immunosuppressant agent inhibiting both T cells and B cells, widely used for the prevention of organ transplant rejection, but also for autoimmune disorders. The first, single-center study showed that mycophenolate mofetil was more effective than intravenous glucocorticoids on moderate-to-severe and active GO, but the experimental design had several limitations (151). The second, large, multicenter study carried out by EUGOGO demonstrated that the combination of mycophenolate sodium and intravenous glucocorticoids was more effective than intravenous glucocorticoids alone (152). The safety profile at the dose used (720 mg/day for 6 months) appears to be good (153). Therefore mycophenolate sodium may represent a useful tool for the management of GO.
Teprotumumab is a monoclonal antibody inhibiting the IGF-1 receptor. Because the latter seems to be involved in the pathogenesis of GO (154), teprotumumab might play a role in the management of the disease. A recent placebo-controlled randomized clinical trial showed that teprotumumab is more effective than placebo in reducing the CAS (155). The most striking effect was marked reduction in the exophthalmos (155), a feature of GO which is very poorly modified by whatever medical treatment. This study is not devoid of limitations and further studies are warranted before it can be included among the tools for the management of active and moderate-to-severe GO (156).
Orbital decompression is a milestone in the management of GO. It is aimed at increasing the space available for the increased orbital content by removing part of the bony walls of the orbit and/or the orbital fibroadipose tissue (157). It is indicated in patients who have impending sight loss due to optic neuropathy and do not respond promptly to intravenous glucocorticoids (157). Other important indications for decompressive surgery are represented by corneal damage due to eyeball exposure in patients with marked proptosis, or by recurrent subluxation of the globe, which may stretch the optic nerve and cause sight loss (157). In recent years, thanks to the improved surgical techniques and the diminished surgical risk, the indications for orbital decompression have expanded, including also correction of residual cosmetic problems (157, 158). Several techniques of orbital decompression are available, aimed at removing part of one, two, three or four orbital walls (floor, roof, lateral wall, medial wall) as well as part of the retroorbital fibroadipose tissue. The different surgical options should be discussed with the patient, as well possible complications of the procedure, particularly the de novo occurrence or worsening of diplopia, particularly frequent after extensive removal of the orbital floor (157, 159). Removal of fibroadipose tissue can be done together with or without bone removal, but removal of fat alone is associated with a lower reduction of proptosis (159).
Rehabilitative surgery includes surgery for strabismus or eyelid retraction. Extraocular muscle surgery is aimed at correcting residual diplopia after medical and/or surgical treatment of GO. Timing of surgery is crucial, because it should not be performed when GO is active, but when it has been inactive for 6 months (160, 161). The goal of eye muscle surgery is to align the eyes, avoiding abnormal head posture and restoring single binocular vision in primary and reading positions; multiple operations may be required to achieve this goal. Eyelid surgery may rarely be an emergency procedures in patients with exposure keratitis and corneal ulcerations, but it usually is carried out to correct eyelid malposition after medical treatment or orbital decompression. Eyelid surgery usually constitutes the last step of rehabilitation (161).
Thyroid ablation. The question of whether in a patient with GO, Graves’ hyperthyroidism should be treated by non-ablative (i.e., thionamides) or ablative (i.e., radioiodine therapy, thyroidectomy, both) therapy is unanswered (162, 163). Supporters of thyroid ablation justify this approach by mentioning the pathogenic link between thyroid and orbit: removal of thyroid-orbit shared antigen(s) and autoreactive T lymphocytes might be beneficial to the eye (162); supporters of non-ablative thyroid treatment suggest that control of thyrotoxicosis by antithyroid drugs may be associated with a reduction of autoimmune phenomena which might be reflected by an amelioration of ocular conditions; furthermore, once triggered, GO might proceed independently of thyroid treatment (163). Two retrospective studies showed that total thyroid ablation (thyroidectomy followed by radioiodine therapy, as in thyroid cancer) was associated with an improvement of clinical GO (164, 165). A recent randomized, controlled clinical trial demonstrated that, as compared to total thyroidectomy alone, total thyroid ablation is followed by a better outcome of GO in patients given intravenous glucocorticoids (166). A follow-up study of this cohort recently showed that in the long run total thyroid ablation was no better than total thyroidectomy alone, although it was associated with a prompter achievement of the best possible result obtainable by medical treatment and with an earlier possibility to submit the patient to rehabilitative surgery (147). Other cohort studies emphasized the opportunity to postpone definitive treatment of hyperthyroidism until GO is cured (168, 169). Thus, the optimal thyroid treatment in patients with GO still is a dilemma (170-172).
THYROID DERMOPATHY AND ACROPACHY
Thyroid dermopathy (also called pretibial myxedema or localized myxedema) is an uncommon extrathyroidal manifestations of Graves’ disease (less frequently of chronic autoimmune thyroiditis) (13, 173). It almost always occurs in Graves’ patients who also have GO. In a review of 178 consecutive patients with thyroid dermopathy, only 4 patients had no evidence of eye disease (174). However, in a community-based epidemiologic study, only 4% of GO patients also had thyroid dermopathy, although the latter was more frequent in patients with severe GO (175). It is more common in older than in younger patients, with a large preponderance in women (176). Skin lesions are edematous and thickened plaques, typically localized in the pretibial area; however they can be less frequently found in other skin areas, such as feet, toes, upper extremities, shoulders, upper back, nose. Prevalent localization in the pretibial area is related to mechanical and dependent position. The occurrence of lesions in less common sites is often preceded (triggered?) by local trauma (177, 178). There can be three clinical types: nodular, diffuse, and elephantias-like.(179, 180) (Figures 7-9).

Fig. 7: Thyroid dermopathy. Courtesy of Dr. Vahab Fatourechi, Mayo Clinic

Fig. 8: thyroid dermopathy. Courtesy of Dr. Vahab Fatourechi, Mayo Clinic

Histopathologically, skin lesions are characterized by the accumulation of activated fibroblasts (and, to a lesser extent, mast cells), with a markedly increased production of glycosaminoglycans in the dermis and subcutaneous tissues (181). Whereas in normal skin approximately 5% of the acid mucopolysaccharides are hyaluronic acid, in pretibial myxedema this amount increases to 90%. Glycosaminoglycans are responsible for fluid retention, subsequent compression and occlusion of lymphatic vessels, and lymphedema (182). Thus, as in GO, fibroblasts seem to play a central role in the pathogenesis of localized myxedema. This notion is further supported by the finding of limited variability of T cell receptor V gene usage in pretibial myxedema, pointing to a primary immune response of antigen-specific T lymphocytes (183). Furthermore, as is the case with acropachy, lymphocytes do recognize local fibroblasts. IgG from patients with pretibial myxedema was shown to stimulate proteoglycan synthesis by human skin fibroblasts (182). As for GO, TSH-R has been implicated in the pathogenesis of localized myxedema. TSH-R is expressed in peripheral skin fibroblasts from patients with localized myxedema, both at the mRNA and protein level (13). However, TSHR is expressed also in skin from normal subjects (183, 184). Likewise, TSH-R immunoreactivity was detected in cultured fibroblasts from pretibial myxedema, although the specificity of this finding remains to be established. As mentioned above, IgG from Graves’ patients with localized myxedema was reported to stimulate glycosaminoglycan production in cultured skin fibroblasts (183), but this data is not unequivocal, because IgG from normal subjects were equally effective in other studies (185). To summarize, although pathogenic mechanisms remain to be fully elucidated, localized myxedema appear to result from autoimmune reactions leading to fibroblast proliferation and increased glycocosaminoglycan secretion.
From a clinical standpoint, localized myxedema presents as light-colored (sometimes yellowish brown) skin lesions, frequently with an orange peel texture (Figures 7-9). Skin lesions may be characterized by hyperpigmentation and hyperkeratosis. They usually represent only a cosmetic problem and are asymptomatic, but sometimes they may be associated with itching and pain, or may be functionally important, e.g., they may cause problems to wear shoes, especially the elephantiasic form of localized myxedema. Localized myxedema may remain stable, but frequently improves with time, partially or completely (13). Many cases of mild localized myxedema do not require any treatment, but in moderately severe lesions or when there is cosmetic concern, topical glucocorticoids applied with occlusive plastic dressing produce beneficial effects in a relevant proportion of patients (13). If necessary, treatment is repeated until clinical remission occurs (13). When localized mxedema is severe and extensive, steroid pulse therapy, or decongestive physiotherapy, a combination of manual lymphatic drainage, bandaging, exercise, and scrupulous skin care, may be tried (13). No substantial effect was reported by long-term octreotide treatment in three patients with localized myxedema (186). Two studies on the use of intravenous IgG in a small number of patients have reported discrepant effects (reviewed in 13). Thus, measures such as compression bandaging and topical glucocorticoids still are the most cost effective treatments for localized myxedema.
Acropachy is a very uncommon extrathyroidal expression of Graves’ disease, usually associated with severe GO (13) and localized myxedema (13), thus reflecting severity of the autoimmune process. It seems more common in women than in men (13). It is characterized by clubbing of fingers (Fig. 10) and toes, with concomitant soft-tissue swelling of hands and feet. These abnormalities are usually painless and may be asymmetric (13). As for GO, there seems to be a strong relation with cigarette smoking. X-ray of affected sites shows soft-tissue swelling and subperiosteal bone formation. There is currently no treatment that can solve the esthetic and (less frequent) functional abnormality of thyroid acropachy, which occasionally may remit spontaneously in the long-term.

Fig. 10: Thyroid acropachy. Courtesy of Dr. Vahab Fatourechi, Mayo Clinic
CLINICAL ABNORMALITIES OF THE HEART
The biochemical actions of thyroid hormone on the heart are described in Chapter 10.
Hyperthyroidism is usually associated with relevant cardiovascular symptoms and changes in cardiovascular hemodynamics (186, 187).Thyrotoxicosis increases the demands on the heart both by chronotropic and inotropic alterations. Cardiac output is markedly increased owing to increased stroke volume and rapid heart rate (186, 187). It is possible that the metabolic efficiency of heart muscle is decreased (186, 187). Irritability of the heart is increased. Investigation with stress echocardiography shows in hyperthyroidism impaired chronotropic, contractile, and vasodilatatory cardiovascular reserves, that are reversible upon conversion to euthyroidism (188). In a recent, large, matched case-control study, cardiovascular symptoms and signs, including palpitations, chest pain, dyspnea, cough, orthopnea, displaced apex, cardiac murmur, chest wheeze/crepitus were much more frequent in hyperthyroid patients than in controls, and some of them persisted despite effective restoration of euthyroidism by antithyroid drug treatment (182). This common finding of cardiovascular alterations in hyperthyroid patients may result from thyroid hormone excess itself, by hyperthyroidism-related worsening of preexisting cardiovascular disorders, or by the occurrence of novel cardiovascular abnormalities (186, 187). The importance of cardiovascular abnormalities is underscored by the observation that mortality of hyperthyroid patients is increased, mainly due to cardiovascular events (189, 190). Similar conclusions were reached also in a community-based study of elderly people (191), in which, however, definition of hyperthyroidism was based on the finding of low/suppressed serum TSH, which may not necessarily reflect thyroid hormone excess, but rather be the result of non-thyroidal illness syndrome.
Mitral valve prolapse was found more commonly in hyperthyroid patients (43%) than in controls (18%) (190). This increased incidence might be due to increased adrenergic tone, autoimmunity, or the augmented cardiac output associated with thyrotoxicosis. Most patients with thyrotoxicosis are adults. Many, especially those with toxic nodular goiter, are in the 50- to 70-years age group, which has a relatively high incidence of organic heart disease anyway (192). Thus, it is not surprising that cardiac abnormalities are prominent among the symptoms of thyrotoxicosis. Frequent premature beats and paroxysmal tachycardia sometimes appear in thyrotoxic patients and may be disturbing to the patient. Atrial fibrillation occurs in thyrotoxicosis with or without preexisting heart disease, but it is more frequent in older patients (193), probably reflecting an increase in the prevalence of underlying cardiac abnormalities of ischemic or different origin (194). It may be paroxysmal or persistent during the thyrotoxic period. Attempts to correct this arrhythmia to normal in patients with persistent atrial fibrillation are usually unsuccessful while they are hyperthyroid. Once euthyroidism has been restored, atrial fibrillation may revert spontaneously or may be converted pharmacologically or by electroconversion. About two-thirds of patients undergo spontaneous reversion to sinus rhythm after receiving therapy for thyrotoxicosis, usually within 4 months; later on, spontaneous conversion is unlikely (195). It is wise to always evaluate thyroid function in clinically euthyroid patients with atrial arrhythmias with or without heart disease, because in about 20% of patients TSH tests and/or FT4 point to an overactive thyroid and in 50% of these patients normal sinus rhythm resumes after treatment with antithyroid drugs (195). It is widely accepted that subclinical hyperthyroidism is associated, in individuals aged 60 years or more with a 3-to-5-fold increased risk of developing atrial fibrillation (195).
Congestive heart failure is a frequent complication in thyrotoxic patients with pre-existing organic heart disease, particularly if old (196-198). In the elderly hyperthyroid patient, cardiac symptoms may so dominate the clinical picture that diagnosis of thyrotoxicosis may be overlooked. Careful attention should be given to this possibility in all patients with congestive heart failure, especially if goiter is detected (196). Congestive heart failure may occur in patients who have no detectable preexisting organic heart disease (199). Overt hyperthyroidism may cause ventricular dilatation and persistent tachycardia, which may lead to heart failure and fatal events (200). It is often difficult to establish whether an underlying heart disease is present in a hyperthyroid patient who also has a disorder of rhythm, a cardiac murmur, or congestive heart failure, because all these conditions may be ascribed to thyrotoxicosis per se. It is frequently gratifying to observe normalization of cardiac findings once euthyroidism has been restored.
In hyperthyroidism, owing to the increased metabolic demand, angina can be worsened if pre-existing, or induced de novo (186, 201, 202). Evidence of myocardial lactate production when the heart is paced at an accelerated rate (203), and normal coronary arteries are found at angiography after episodes of angina or infarction (203), have suggested that changes in thyrotoxicosis are due to an imbalance between O2 demand and supply rather than to arterial obstruction. This possibility is corroborated by the finding that coronary artery spasm of an otherwise normal vessel may occur during thyrotoxicosis (202).
Cardiac abnormalities found in Graves' disease often are entirely reversible, except that longstanding atrial fibrillation due to hyperthyroidism is not always convertible after euthyroidism is restored. It has become evident that even in the mildest forms of thyrotoxicosis subtle cardiac abnormalities may be present. Thus, in patients with so-called "subclinical" thyrotoxicosis, i.e. suppressed TSH and normal serum free T4 and T3 concentrations, due to multinodular, autonomous goiter or TSH-suppressive T4 treatment, mean basal 24-h heart rate is increased, there is an augmented risk of atrial premature beats and atrial fibrillation, and left ventricular function and wall thickness are increased (204).There is controversy whether TSH suppressive T4 treatment leads to functional cardiac abnormalities (204, 205).
Treatment of heart failure in the presence of thyrotoxicosis does not differ from its treatment in euthyroid patients, but it may be more difficult. Rest, salt restriction, diuretic therapy, digitalization and administration of afterload-reducers, like angiotensin converting enzyme (ACE) inhibitors, betablockers, aldosterone antagonists and other specific measures, are in order (186, 196). Larger than normal doses of digoxin are required, but there is probably no change in the toxic-to-therapeutic dose ratio. Atrial fibrillation may be controlled by digoxin, propranolol, or both. Electroconversion is usually successful only after thyrotoxicosis has been resolved for a few months (206).
Hyperthyroidism should be controlled as expeditiously as possible. Congestive heart failure is a contraindication to operation. Most patients with thyrotoxicosis and clinically relevant heart disease are now treated with RAI. This treatment may be preceded by a 3-to-6-month course of antithyroid drug therapy to deplete their glands of stored thyroid hormone, a program that lessens any chance of an exacerbation of the heart disease caused by a radioiodine-induced release of thyroid hormone from the gland. Administration of 131I followed by antithyroid drugs, and potassium iodide or ipodate, that also inhibit T4 to T3 conversion, may be used in severely ill patients in whom a prompt response is needed. This method is described in Chapter 11.
Propranolol has been used successfully in the control of tachycardia, and also in patients with congestive heart failure if tachycardia appeared to be adding substantially to the problem. In these instances, possible depression of myocardial contractility by the drug was outweighed by the benefit derived from controlling the rate. In such circumstances, one must proceed with caution and often digoxin should be added.
References
- Klubo-Gwiezdzinska J, Wartoksky L 2012 Thyroid emergencies. Med Clin North Am 96: 385-403.
- Carroll R, Matfin G 2010 Endocrine and metabolic emergencies: thyroid storm. Ther Adv Endocrinol Metab 1: 139-145.
- Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T et al. 2012 Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 22: 661-679
- Akamizu T 2018 Thyroid storm: a Japanese perspective. Thyroid 28: 32-40
- Nelson NC, Becker WF 1969 Thyroid crisis: diagnosis and treatment. Ann Surg 170:263-273.
- Kobayashi C, Sasaki H, Kosuge K, Miyakita Y, Hayakawa M, Suzuki A, Abe E, Suzuki K, Aizawa Y.2005 Severe starvation hypoglycemia and congestive heart failure induced by thyroid crisis, with accidentally induced severe liver dysfunction and disseminated intravascular coagulation. Intern Med. 44:234-239.
- McDermott MT, Kidd GS, Dodson LE, Hofeldt FD 1983 Radioiodine-induced thyroid storm. Am J Med 75:353-359.
- Bartalena L 2013 Diagnosis and management of Graves disease: a global overview. Nat Rev Endocrinol 9: 724-734.
- Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, Tsuboi K, Kanamoto N, Otani H, Furukawa Y, Teramukai S, Teramukai S, Akamizu T 2016 2016 guidelines for the management of thyroid storm from the Japan Thyroid Association and Japan Endocrine Society (First edition). Endocrine J 63: 1025-1024.
- Thomas DJ, Hardy J, Sarwar R, Banner NR, Mumani S, Lemon K, Hillson RM 2006 Thyroid storm treated with intravenous methimazole in patients with gastrointestinal dysfunction. Br J Hosp Med. 67: 492-493.
- Bartalena L, Pinchera A, Marcocci C 2000 Management of Graves’ ophthalmopathy: reality and perspectives. Endocr Rev 21: 168-199.
- Bartalena, Tanda ML 2009 Clinical Practice: Graves’ ophthalmopathy. N Engl J Med 360: 994.1001.
- Bartalena L, Fatourechi V 2014 Extrathyroidal manifestations of Graves’ disease: a 2014 update. J Endocrinol Invest 37: 691-700.
- Smith TJ, Hegedus L 2016 Graves’ disease. N Engl J Med 375: 1552.1575.
- Bartalena L, Chiovato L, Vitti P 2016 Management of hyperthyroidism due to Graves’ disease: frequently asked questions and answers (if any). J Endocrinol Invest 39: 1105-1114.
- Bartley GB 1994 The epidemiological characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc 92: 477-588.
- Tanda ML, Piantanida E, Liparulo L, Veronesi G, Lai A, Sassi L, Pariani N, Gallo D, Azzolini C, Ferrario M, Bartalena L 2013. Prevalence and natural history of Graves’ orbitopathy in a large series of patients with newly diagnosed Graves’ hyperthyroidism seen at a single center. J Clin Endocrinol Metab 98: 1443-1449.
- Laurberg P, Berman DC, Bulow Pedersen I, Andersen S, Carlé A 2012 Incidence and clinical presentation of moderate to severe Graves’ orbitopathy in a Danish population before and after iodine fortification of salt. J Clin Endocrinol Metab 97: 2325-2332.
- Perros P, Hegedus L, Bartalena L, Marcocci C, Kahaly GJ, Baldeschi L et al. 2017 Graves orbitopathy as a are disease in Europe: a European Group on Graves’ Orbitopathy (EUGOGO) position statement. Orphanet J Rare Dis 12: 72.
- Marcocci C, Bartalena L, Bogazzi F, Panicucci M, Pinchera A 1989 Studies on the occurrence of ophthalmopathy in Graves’ disease. Acta Endocrinol (Copenh) 120: 473-478.
- Perros P, Crombie AL, Matthews JNS, Kendall-Taylor P 1993 Age and gender influence the severity of thyroid associated ophthalmopathy: a study of 101 patients attending a combined thyroid-eye clinic. Clin Endocrinol (Oxf) 38: 367-372.
- Perros P, Crombie AL, Kendall-Taylor P 1995 Natural history of thyroid-associated ophthalmopathy. Clin Endocrinol (Oxf) 42: 45-50.
- Kendall-Taylor P, Perros P 1998 Clinical presentation of thyroid associated orbitopathy. Thyroid 8: 427-428.
- Piantanida E, Tanda ML, Lai A, sassi L, Bartalena L 2013 Prevalence and natural history of Graves’ orbitopathy in the XXI century. J Endocrinol Invest 36: 444-449.
- Prummel MF, Bakker A, Wiersinga WM, Baldeschi L, Mourits MP, Kendall-Taylor P, Perros P, Neoh C, Dickinson AJ, Lazarus JH, Lane CM, Heufelder AE, Kahaly GJ, Pitz S, Orgiazzi J, Hullo A, Pinchera A, Marcocci C, Sartini MS, Rocchi R, Nardi M, Krassas GE, Halkias A 2003 Multi-center study on the characteristics and treatment strategies of patients with Graves’ orbitopathy: the first European Group on Graves’ Orbitopathy experience. Eur J Endocrinol 148: 491-495.
- Bartalena L, Masiello E, Magri F, Veronesi G, Bianconi F, Zerbini F et al. 2016 The phenotype of newly diagnosed Graves’ disease in Italy in recent years is milder than in the past: results of a large observational longitudinal study. J Endocrinol Invest 39: 1445-1451
- Anagnostis P, Boboridis K, Adamidou F, Kita M 2017 Natural course of mild Graves’ orbitopathy: is it a chronic remitting or a transient disease? J Endocrinol Invest 40: 257-261.
- Sabini E, Leo M, Mazzi B, Rocchi R, Latrofa F, Nardi M et al. 2017 Does Graves’ orbitopathy ever disappear? Answers to an old question. Eur Thyroid J 6: 263-270.
- Bartalena L, Bogazzi F, Tanda ML, Manetti L, Dell’Unto E, Martino E 1995 Cigarette smoking and the thyroid. Eur J Endocrinol 133: 507.512.
- Wiersinga WM 2013 Smoking and thyroid. Clin Endocrinol (Oxf) 79: 145-151.
- Bartalena L, Martino E, Marcocci C, Bogazzi F, Panicucci M, Velluzzi F, Loviselli A, Pinchera A 1989 More on smoking habits and Graves’ ophthalmopathy. J Endocrinol Invest 12: 733-737.
- Holm IA, Manson JAE, Michels KB, Alexander EK, Willett WC, Utiger RD 2005 Smoking and other lifestyle factors and the risk of Graves’ hyperthyroidism. Arch Intern Med 165: 1606-1611.
- Prummel MF, Wiersinga WM 1993 Smoking and risk of Graves’ disease. JAMA 269: 479-482.
- Krassas GE, Segni M, Wiersinga WM 2005 Childhood Graves’ ophthalmopathy: results of a European questionnaire study. Eur J Endocrinol 153: 515-521.
- Bartalena L, Marcocci C, Pinchera A 2002 Graves’ ophthalmopathy: a preventable disease? Eur J Endocrinol 146: 457-461.
- Szucs-Farkas Z, Todt J, Kollar J, Galuska L, Barman KD, Boda J, Leovey A, Varga J, Ujhelyi B, Szabo J, Berta A, Nagy EV 2005 Volume changes in intra- and extraorbital compartments in patients with Graves’ ophthalmopathy: effect of smoking. Thyroid 15: 146-151.
- Cawood TJ, Moriarty P, O’Farrelly C, O’Shea D 2007 Smoking and thyroid-associated ophthalmopathy: a novel explanation of the bilogical link. J Clin Endocrinol Metab 92: 59-64.
- Khong JJ, Finch S, De Silva C, Rylander S, Cgarig JE, Selva D, Ebeling PR 2016 Risk facrors for Graves’ orbitopathy: the Australian Thyroid-Associated Research (ATOR) study. J Clin Endocrinol Metab 101: 2711-2720.
- Smith TJ 2010 Pathogenesis of Graves’ orbitopathy: a 2010 update. J Endocrinol Invest 33: 414-421.
- Bahn RS 2015 Current insights into the pathogenesis of Graves’ ophthalmopathy. Horm Metab Res 43: 773-776.
- Salvi M, Berchner-Pfannschmidt U, Ludgate M 2017 Pathogenesis. In (Wiersinga WM, Kahaly GJ (Eds.) Graves’ orbitopathy – A multidisciplinary approach: questions and answers. Karger, Basel, pp. 41-60
- Prabhakar BS, Bahn RS, Smith TJ 2003 Current perspective on the pathogenesis of Graves’ disease and ophthalmopathy. Endocr Rev 24: 802-835.
- Potgieser PW, Wiersinga WM, Regensburg NI, Wiersinga WM 2015 Some studies on the natural history of Graves’ orbitopathy: increase in orbital fat is a rather late phenomenon. Eur J Endocrinol 173: 149-153.
- Wang Y, Smith TJ 2014 Current concepts in the molecular pathogenesis of thyroid-associated ophthalmopathy. Invest Ophthalmol Vis Sci 55: 1735-1748.
- Ajjan AR, Weetman AP 2004 New understanding of the role of cytokines in the pathogenesis of Graves’ ophthalmopathy. J Endocrinol Invest 27: 237-245.
- Feldon SE, Park DJJ, O’Loughlin CW, Nguyen VT, Landskroner-Eiger S, Chang D, Thatcher TH, Phipps RP 2005 Autologous T-lymphocytes stimulate proliferation of orbital fibroblasts derived from patients with Graves’ ophthalmopathy. Invest Ophthalmol Vis Sci 46: 3913-3921.
- Khong JJ, McNab AA, Ebeling PR, Craig JR, Silva D 2016 Pathogenesis of thyroid eye disease: review and update on molecular mechanisms. Br J Ophthalomol 100: 142-150.
- Bahn RS 2004 TSH receptor expression in orbital tissue and its role in the pathogenesis of Graves’ ophthalmopathy. J Endocrinol Invest 27: 216-220.
- Agretti P, De Marco G, De Servi M, Marcocci C, Vitti P, Pinchera A, Tonacchera M 2005 Evidence for protein and mRNA expression in fibroblasts from patients with thyroid-associated ophthalmopathy (TAO) after adipocytic differentiation. Eur J Endocrinol 152: 777-784.
- Agretti P, Chiovato L, De Marco G, Marcocci C, Mazzi B, Sellari-Franceschini S, Vitti P, Pinchera A, Tonacchera M 2002 Real-time PCR provides evidence for thyrotropin receptor mRNA expression in orbital as well as in extraorbital tissues. Eur J Endocrinol 147: 733-739.
- Garrity JA, Bahn RS 2006 Pathogenesis of Graves’ ophthalmopathy: implications for prediction, prevention, and treatment. Am J Ophthalmol 142: 147-153.
- Ludgate M, Baker G 2004 Inducing Graves’ ophthalmopathy. J Endocrinol Invest 27: 211-215.
- Moshkelgosha S, So P-W, Deasy N, Diaz-Cano S, Banga JP 2013 Cutting edge: retrobulbar inflammation, adipogenesis, and acute orbital congestion in a preclinical female mouse model of Graves’ orbitopathy induced by thyrotropin receptor plasmid-in vivo electroporation. Endocrinology 154: 3008-3015.
- Banga JP, Moshkelgosha S, Berchner-Pfannschmidt U, Eckstein A 2015 Modeling Graces’ orbitopathy in experimental Graves’ disease. Horm Metab Res 47: 797-803.
- Nagayama Y, Nakahara M, Abiru N 2015 Animal models of Graves’ disease and Graves’ orbitopathy. Current Opin Endocrinol Diabetes Care 22: 381-386.
- Tu Y, Wang Y, Ding L, Zhang Y, Wu W 2016 Development of a novel thyroid function fluctuated animal model for thyroid-associated ophthalmopathy. PLoS One 11: e0148595
- Ungerer M, Fassbender J, Li Z, Munch G, Holthoff H-p 2017 Review of mouse models of Graves’ disease and orbitopathy – Novel treatment by induction of tolerance. Clin Rev Allerg Immunol 52: 182-193.
- Smith TJ, Huetwell FGL, Hegedus L, Douglas RS 2012 Role of insulin-like growth factor-1 (IGF-1) pathway in the pathogenesis of Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab 26: 291-302.
- Weightman DR, Perros P, Sherif IH, Kendall-Taylor P 1993 Autoantibodies to IGF-1 binding sites in the thyroid-associated phthalmopathy. Autoimmunity 16: 251-257
- Tsui S, Naik V, Hoan N, Hwang CJ, Afifiyan NF, Hikim Sinha A, Gianoukakis AG, Douglas RS, Smith TJ 2008 Evidence for an association between thyroid-stimulating hormone and insulin like growth factor 1 receptors: a tale of two antigens implicated in Graves’ disease. J Immunol 181: 4397-4405.
- Kumar S, Iyer S, Bauer H, Coenen M, Bahn RS 2012 A stimulatory thyrotropin receptor antibody enhances hyaluronic acid synthesis in Graves’ orbital fibroblasts: inhibition by an IGF-I receptor blocking antibody. J Clin Endocrinol Metab 97: 1681-1687
- Pritchard J, Tsui S, Horst N, Cruikshank WW, Smith TJ 2004 Synovial fibroblasts from patients with rheumatoid arthritis, like fibroblasts from Graves’ disease, express high levels of IL-16 when treated with Igs against insulin-like growth factor-1 receptor. J Immunol 173: 3564-3569.
- Smith TJ 2013 Is IGF-I receptor a target for autoantibody generation in Graves’ disease? J Clin Endocrinol Metab 98: 515-518.
- Wiersinga WM 2011 Autoimmunity in Graves’ ophthalmopathy: the result of an unfortunate marriage between TSH receptors and IGF-1 receptors? J Clin Endocrinol Metab 96: 2386-2394.
- Minich WB, Dehina N, Welsink T, Schwiebert C, Morgenthaler NG, Kohrle J, Eckstein A, Schomburg L 2013 Autoantibodies to the IGF1 receptor in Graves’ orbitopathy. J Clin Endocrinol Metab 98: 752-760.
- Varewijck AJ, Boelen A, Lamberts SJ, Fliers E, Jofland LJ, Wiersinga WM, Janssen JAMJL 2013 Circulating IgGs may modulate IGF-I receptor stimulating activity in a subset of patients with Graves’ ophthalmopathy. J Clin Endocrinol Metab 98: 769-776.
- Song D, Wang R, Zhong Y, Li W, Li H, Dong F 2012 Locally produced insulin-like growth factor-1 by orbital fibroblasts as implicative pathogenic factor rather than systemically circulated IGF-1 for patients with thyroid-associated ophthalmopathy. Graefes Arch Clin Exp Ophthalmol 250: 433-440.
- Bartalena L 2005 Graves’ ophthalmopathy: search for shared autoantigen(s) continues. J Endocrinol Invest 28: 396-397.
- Vaidya B, Kendall-Taylor P, Pearce SHS 2002 The genetics of autoimmune thyroid disease. J Clin Endocrinol Metab 87: 5385-5397.
- Brand OJ, Gough SCL 2010 Genetics of thyroid autoimmunity and the role of the TSHR. Mol Cell Endocrinol 322: 135-143.
- Brix TH, Hegedus L 2012 Twin studies as a model for exploring the aetiology of autoimmune thyroid disease. Clin Endocrinol (Oxf) 76: 457-464.
- Tomer Y 2014 Mechanisms of autoimmune thyroid diseases: from genetics to epigenetics. Annu Rev Pathol 9: 147-156.
- Marinò M, Latrofa F, Menconi F, Chiovato L, Vitti P 2015 Role of genetic and non-genetic factors in the etiology of Graves’ disease. J Endocrinol Invest 38: 283-294.
- Tomer Y 2010 Genetic susceptibility to autoimmune thyroid disease: past, present, future. Thyroid 20: 715-725.
- Yin X, Latif R, Bahn RS, Davies TF 2012 Genetic profiling in Graves’ disease: further evidence for lack of a distinct genetic contribution to Graves’ orbitopathy. Thyroid 22: 730-735.
- Juriecka-Lubieniecka B, Ploski R, Kula D et al 2014 Association between polymorphisms in the TSHR gene and Graves’ orbitopathy 2014 PLoS One 9: e102653
- Bartalena L 2012 Prevention of Graves’ ophthalmopathy. Best Pract Res Clin Endocrinol Metab 26: 371-379.
- Prummel MF, Wiersinga WM, Mourits MP, Koornneef L, Berghout A, van der Gaag R. 1989 Amelioration of eye changes of Graves’ ophthalmopathy by achieving euthyroidism. Acta Endocrinol (Copenh) 121: 185-189.
- Prummel MF, Wiersinga WM, Mourits MP, Koornneef L, Berghout A, van der Gaag R. 1990 Effect of abnormal thyroid function on the severity of Graves’ ophthalmopathy. Arch Intern Med 150: 1098-1101.
- Karlsson AF, Westermark K, Dahlberg PA, Jansson R, Enksson P 1989 Ophthalmopathy and thyroid stimulation. Lancet 2: 691.
- Eckstein AK, Plicht M, Lax H, Neuhauser M, Mann K, Lederbogen S, Heckmann C, Esser J, Morgenthaler NG 2006 Thyrotropin receptor autoantibodies are independent risk factors for Graves’ ophthalmopathy and help to predict severity and outcome of the disease. J Clin Endocrinol Metab 91: 3464-3470.
- Tallstedt L, Lundell G, Torring O, Wallin G, Ljunggren J-G, Blomgren H, Taube A & the Thyroid Study Group. 1992 Occurrence of ophthalmopathy after treatment for Graves’ hyperthyroidism. N Engl J Med 326: 1733-1738.
- Bartalena L, Marcocci C, Bogazzi F, Manetti L, Tanda ML, Dell’Unto E, Bruno-Bossio G, Nardi M, Bartolomei MP, Lepri A, Rossi G, Martino E, Pinchera A 1998 Relation between therapy for hyperthyroidism and the course of Graves’ ophthalmopathy. N Engl J Med 338: 73-78.
- Traisk F, Tallstedt L, Abraham-Nordling M, Andersson T, Berg G, Calissendorff J, Hallengren B, Hdner P, Lantz M, Nystrom E, Ponjavic V, Taube A, Torring O, Wallin G, Asman P, Lundell G 2009 Thyroid-associated ophthalmopathy after treatment for Graves’ hyperthyroidism with antithyroid drugs or iodine-131. J Clin Endocrinol Metab 94: 3000-3007.
- Acharya SH, Avernell A, Philip S, Burr J, Bevan JS, Abraham P 2008 Radioiodine therapy (RAI) for Graves’ disease (GD) and the effect on the ophthalmopathy: a systematic review. Clin Endocrinol (Oxf) 69: 943-950.
- Li HX, Xiang N, Hu WK, Jiao XL 2016 Relation between therapy options for Graves’ disease and the course of Graves’ ophthalmopathy: a systematic review and meta-analysis. J Endocrinol Invest 38: 1225-1233.
- Bartalena L, Marcocci C, Bogazzi F, Panicucci M, Lepri A, Pinchera A 1989 Use of corticosteroids to prevent progression of Graves’ ophthalmopathy after radioiodine therapy for hyperthyroidism. N Engl J Med 321: 1349-1352.
- Lai A, Sassi L, Compri E, Marino F, Sivelli P, Piantanida E, Tanda ML, Bartalena L 2010 Lower dose prednisone prevents radioiodine-associated exacerbation of initially mild or absent Graves’ orbitopathy: a retrospective cohort study. J Clin Endocrinol Metab 95: 1333-1337.
- Bartalena L, Baldeschi L, Dickinson A, Eckstein A, Kendall-Taylor P, Marcocci C, Mourits M, Perros P, Boboridis K, Boschi A, Currò N, Daumerie C, Kahaly GJ, Krassas GE, Lane CM, Lazarus JH, Marinò M, Nardi M, Neoh C, Orgiazzi J, Pearce S, Pinchera A, Pitz S, Salvi M, Sivelli P, Stahl M, von Arx G, Wiersinga WM 2008 Consensus statement of the European Group on Graves’ Orbitopathy (EUGOGO) on management of GO. Eur J Endocrinol 158: 273-285.
- Bartalena L, Baldeschi L, Dickinson J, Eckstein A, Kendall-Taylor P, Marcocci C, Mourits M, Perros P, Boboridis K, Boschi A, Currò N, Daumerie C, Kahaly GJ, Krassas GE, Lane CM, Lazarus JH, Marinò M, Nardi M, Neoh C, Orgiazzi J, Pearce S, Pinchera A, Pitz S, Salvi M, Sivelli P, Stahl M, von Arx G, Wiersinga WM 2008 Consensus statement of the European Group on Graves’ Orbitopathy (EUGOGO) on management of Graves’ Orbitopathy. Thyroid 18: 333-346.
- Marcocci C, Bruno-Bossio G, Manetti L, Tanda ML, Miccoli P, Iacconi P, Bartolomei MP, Nardi M, Pinchera A, Bartalena L 1999 The course of Graves’ ophthalmopathy is not influenced by near-total thyroidectomy. Clin Endocrinol (Oxf) 51: 503-508.
- Bartalena L, Baldeschi L, Boboridis K et al 2016 The 2016 European Thyroid Association/European Group on Graves’ Orbitopathy guidelines for the management of Graves’ orbitopathy. Eur Thyroid J 5: 9-26.
- Werner SC 1977 Modification of the classification of the eye changes of Graves’ disease: recommendations of the ad hoc committee of the American Thyroid Association. J Clin Endocrinol Metab 44: 203-206.
- The European Group on Graves’ Orbitopathy (EUGOGO): Wiersinga WM, Perros P, Kahaly GJ, Mourits MP, Baldeschi L, Boboridis K, Boschi A, Dickinson AJ, Kendall-Taylor P, Krassas GE, Lane CM, Lazarus JH, Marcocci C, Marinò M, Nardi M, Neoh C, Orgiazzi J, Pinchera A, Pitz S, Prummel MF, Sartini MS, Stahl M, von Arx G 2006 Clinical assessment of patients with Graves’ orbitopathy: the European Group on Graves’ Orbitopathy recommendations to generalists, specialists and clinical researchers. Eur J Endocrinol 155: 387-389.
- Dolman PJ 2012 Evaluating Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab 26: 229-248.
- Dickinson AJ, Perros P 2001 Controversies in the clinical evaluation of thyroid-associated orbitopathy: use of a detailed protocl with comparative photographs for objective assessment. Clin Endocrinol (Oxf) 55: 283-303.
- McKeag D, Lane C, Lazarus JH, Baldeschi L, Boboridis K, Dickinson AJ. Hullo AI, Kahaly G, Krassas G, Marcocci C, Marinò M, Mourits MP, Nardi M, Neoh C, Orgiazzi J, Perros P, Pinchera A, Pitz S, Plummer MF, Sartini MS, Wiersinga WM 2007 Clinical features of of dysthyroid optic neuropathy: a European Group on Graves’ Orbitopathy (EUGOGO) survey. Br J Ophthalmol 91: 455-458.
- Wiersinga WM 2017 Quality of life. In Wiersinga WM, Kahaly GJ (eds), Graves’ orbitopathy. A multidisciplinary approach – Questions and answers, Karger, Basel, 3rd ed., 260-274.
- Gerding MN, Terwee CB, Dekker FW, Koornneef L, Prummel MF, Wiersinga WM 1997 Quality of life in patients with Graves’ ophthalmopathy is markedly decreased: measurement by the Medical Outcomes Study instrument. Thyroid 7: 885-889.
- Terwee CB, Gerding MN, Dekker FW, Prummel MF, Wiersinga WM 1998 Development of a disease-sepcific quality of life questionnaire for patients with Graves’ ophthalmopathy. Br J Ophthalmol 82: 773-779.
- Kahaly GJ, Petrak F, Hardt J, Pitz S, Egle UT 2005 Psychosocial morbidity of Graves’ orbitopathy. Clin Endocrinol (Oxf) 63: 395-402.
- Terwee CB, Dekker FW, Mourits MP, Gerding MN, Baldeschi L, Kalmann R, Prummel MF, Wiersinga WM 2001 Interpretation and validity of changes in scores in the GO-QOL after different treatments. Clin Endocrinol (Oxf) 54: 391-398.
- Terwee CB, Dekker FW, Mourits MP, Gerding MN, Baldeschi L, Kalmann R, Prummel MF, Wiersinga WM 2001 Interpretation and validity of changes in scores in the GO-QOL after different treatments. Clin Endocrinol (Oxf) 54: 391-398.
- Mourits M, Koornneef L, Wiersinga WM, Prummel MF, Berghout A, van der Gaag R 1989 Clinical criteria for the assessment of disease activity in Graves’ ophthalmopathy: a novel approach. Br J Ophthalmol 73: 639-644.
- Pinchera A, Wiersinga WM, Glinoer D, Kendall-Taylor P, Koornneef L, Marcocci C, Schleusener H, Romaldini J, Niepominiscze F, Solomon D, Garrity J, Gorman CA 1992 Classification of eye changes of Graves’ disease. Thyroid 2: 235-236.
- Pitz S, Muller-Forell W 2017 Orbital imaging. In Wiersinga WM, Kahaly GJ (eds), Graves’ orbitopathy. A multidisciplinary approach – Questions and answers, Karger, Basel, 3rd ed., 61-73.
- Bartalena L, Chiovato L 2014 Graves’-like orbitopathy: do not forget IgG4-related disease. J Endocrinol Invest 37: 1233-1235.
- The European Group of Graves’ Orbitopathy: Perros P, Baldeschi L, Boboridis K, Dickinson AJ, Hullo A, Kahaly GJ, Kendall-Taylor P, Krassas GE, Lane CM, Lazarus JH, Marcocci C, Marinò M, Mourits MP, Nardi M, Orgiazzi J, Pinchera A, Pitz S, Prummel MF, Wiersinga WM 2006 A questionnaire survey on the management of Graves’ orbitopathy in Europe. Eur J Endocrinol 155: 207-211.
- Bartalena L, Marcocci C, Pinchera A. 1997 Treating severe Graves’ ophthalmopathy. Bailliere’s Clin Endocrinol Metab 11: 521-536
- Tanda ML, Piantanida E, Liparulo L, Veronesi G, Lai A, Sassi L, Pariani N, Gallo D, Azzolini C, Ferrario M, Bartalena L 2013 Prevalence and natural hostory of Graves’ orbitopathy in a large series of patients with newly diagnosed Graves’ hyperthyroidism seen at a single center. J Clin Endocrinol Metab 98: 1443-1449.
- Bartalena L, Masiello E, Magri F et al. 2016 The phenotype of newly diagnosed Graves’ disease in Italy in recent years is milder than in the past: results of a large observational longitudinal study. J Endocrinol Invest 39: 1445-1451.
- Boboridis K, Anagnostis P 2017 Local treatment modalities. In Wiersinga WM, Kahaly GJ (eds), Graves’ orbitopathy. A multidisciplinary approach – Questions and answers, Karger, Basel, 3rd ed., 202-206.
- Pfeilschifter J, Ziegler R 1996 Smoking and endocrine ophthalmopathy: impact of smoking severity and current vs lifetime cigarette consumption. Clin Endocrinol (Oxf) 45: 477-481.
- Marcocci C, Kahaly GJ, Krassas GE, Bartalena L, Prummel M, Stahl M, Altea MA, Nardi M, Pitz S, Boboridis K, Sivelli P, von Arx G, Mourits MP, Baldeschi L, Bencivelli W, Wiersinga W and the European Group on Graves’ Orbitopathy 2011 Selenium and the course of mild Graves’ orbitopathy. N Engl J Med 364: 1920-1931.
- Marcocci C, Bartalena L 2013 Role of oxidative stress and selenium in Graves’ hyperthyroidism and orbitopathy. J Endocrinol Invest 36 (suppl. to no. 10): 15-20.
- Bartalena L, Marcocci C, Tanda ML, Piantanida E, Lai A, Marinò M, Pinchera A 2005 An update on medical management of Graves’ ophthalmopathy. J Endocrinol Invest 28: 469-478.
- Zang S, Ponto KA, Kahaly GJ 2011 Intravenous glucocorticoids for Graves’ orbitopathy: efficacy and morbidity. J Clin Endocrinol Metab 96: 320-332.
- Ebner R, Devoto MH, Weil D, Bordaberry M, Mir C, Martinez H, Bonelli L, Niepomniszcze H 2004 Treatment of thyroid associated ophthalmopathy with periocular injections of triamcinolone. Br J Ophthalmol 88: 1380-1386.
- Bartalena L 2005 Glucocorticoids for Graves’ ophthalmopathy: how and when. J Clin Endocrinol Metab 90: 5497-5499
- Marcocci C, Bartalena L, Tanda ML, Manetti L, Dell’Unto E, Rocchi R, Barbesino G, Mazzi B, Bartolomei MP, Lepri P, Cartei F, Nardi M, Pinchera A 2001 Comparison of the effectiveness and tolerability of intravenous or oral glucocorticoids associated with orbital radiotherapy in the management of severe Graves’ ophthalmopathy: results of a prospective, single-blind, randomized study. J Clin Endocrinol Metab 86: 3562-3567.
- van Geest RJ, Sasim IV, Koppeschaar HPF, Mourits MP 2008 Methylprednisolone pulse therapy for patients with moderately severe Graves’ orbitopathy: a prospective, randomized, placebo-controlled study. Eur J Endocrinol 158: 229-237.
- Marinò M, Morabito E, Brunetto MR, Bartalena L, Pinchera A, Marcocci C 2004 Acute and severe liver damage associated with intravenous glucocorticoid pulse therapy in patients with Graves’ ophthalmopathy. Thyroid 14: 403-406.
- Sabini E, Sisti E, Coco B, Leo M, Ionni I, Menconi F et al 2016 Statins are not a risk factor for liver damage associated with intravenous glucocorticoid pulse therapy for Graves’ orbitopathy. J Endocrinol Invest 39: 1323-1327.
- Kahaly GJ, Pitz S, Hommel G, Dittmar M 2005 Randomized, single blind trial of intravenous versus oral steroid monotherapy in Graves’ orbitopathy. J Clin Endocrinol Metab 90: 5234-5240.
- Marcocci C, Watt T, Altea MA, Rasmussen AK, Feldt-Rasmussen U, Orgiazzi J, Bartalena L and the European Group on Graves’ Orbitopathy 2012 Fatal and non-fatal adverse events of glucocorticoid therapy for Graves’ orbitopathy: a questionnaire survey among members of the European Thyroid Association. Eur J Endocrinol 166: 247-253.
- Bartalena L, Krassas GE, Wiersinga W, Marcocci C, Salvi M, Daumerie C, Bournaud C, Stahl M, Sassi L, Veronesi G, Azzolini C, Boboridis KG, Mourits MP, Soeters MR, Baldeschi L, Nardi M, Currò N, Boschi A, Bernard M, von Arx G and the European Group on Graves’ Orbitopathy 2012 Efficacy and safety of three different cumulative doses of intravenous methylprednisolone for moderate to severe and active Graves’ orbitopathy. J Clin Endocrinol Metab 97: 4454-4463
- Bartalena L, Veronesi G, Krassas GE, Wiersinga WM, Marcocci C, Marinò M et al 2017 Does early response to intravenous glucocorticoids predict the final out come in patients with moderate-to-severe and active Graves’ orbitopathy? J Endocrinol Invest 40: 547-553.
- Zang S, Ponto KA, Kahaly GJ 2011 Dose of intravenous steroids and therapy outcome in Graves’ orbitopathy. J Endocrinol Invest 34: 876-880.
- Jespersen S, Nygaard B, Ostergaard Kristensen L 2015 Methyprednisolone pulse treatment of Graves’ ophthalmopathy is not associated with secondary adrenocortical insufficiency. Eur Thyroid J 4: 222-225.
- Giotaki Z, Fountas A, Tsirouki T, Bargiota A, Tigas S, Tsatsoulis A 2015 Adrenal reserve following treatment of Graves’ orbitopathy with intravenous glucocorticoids. Thyroid 25: 462-463.
- Tanda ML, Bartalena L 2012 Efficacy and safety of orbital radiotherapy for Graves’ orbitopathy. J Clin Endocrinol Metab 97: 3857-3865.
- Kahaly GJ, Rosler H-P, Pitz S, Hommel G 2000 Low- versus high-dose radiotherapy for Graves’ ophthalmopathy: a randomized, single blind trial. J Clin Endocrinol Metab 85: 102-108.
- Bartalena L, Marcocci C, Gorman CA, Wiersinga WM, Pinchera A 2003 Orbital radiotherapy for Graves’ ophthalmopathy: useful or useless? Safe or dangerous. J Endocrinol Invest 26: 5-16.
- Bradley EA, Gower EW, Bradley DJ, Meyer DR, Cahill KV, Custer PL, Holck DE, Woog JJ 2008 Orbital radiation for Graves ophthalmopathy. Ophthalmology 115: 398-409.
- Prummel MF, Mourits MP, Blank L, Berghout A, Koornneef L, Wiersinga WM 1993 Randomised, double-blind trial of prednisone versus radiotherapy in Graves’ ophthalmopathy. Lancet 342: 949-954.
- Mourits MP, van Kempen-Harteveld ML, Garcia MB, Koppeschaar HPF, Tick L, Terwee CB 2000 Radiotherapy for Graves’ orbitopathy: randomised, placebo-controlled study. Lancet 355: 1505-1509.
- Gorman CA, Garrity JA, Fatourechi V, Bahn RS, Petersen IA, Stafford SL, Earle JD, Forbes GS, Kline RW, Bergstrahl EJ, Offord KP, Rademacher DM, Stanley NM, Bartley GB 2001 A prospective, randomized, double-blind, placebo-controlled study of orbital radiotherapy for Graves’ ophthalmopathy. Ophthalmology 108: 1523-1534.
- Prummel MF, Terwee CB, Gerding MN, Baldeschi L, Mourits MP, Blank L, Dekker FW, Wiersinga WM 2004 A randomized controlled trial of orbital radiotherapy versus sham irradiation in patients with mild Graves’ ophthalmopathy. J Clin Endocrinol Metab 89: 15-20.
- Marcocci C, Bartalena L, Rocchi R, Marinò M, Menconi F, Morabito E, Mazzi B, Mazzeo S, Sartini MS, Nardi M, Cartei F, Cionini L, Pinchbera A 2003 Long-term safety of orbital radiotherapy for Graves’ ophthalmopathy. J Clin Endocrinol Metab 88: 3561-3566.
- Wakelkamp IMMJ, Tan H, Saeed P, Sckingemann RO, Verbraak FD, Blank LECM, Prummel MF, Wiersinga WM 2004 Orbital irradiation for Graves’ ophthalmopathy. Is it safe? A long-term follow-up study. Ophthalmology 111: 1557-1562.
- Bartalena L, Marcocci C, Chiovato L, Laddaga M, Lepri G, Andreani D, Cavallacci G, Baschieri L, Pinchera A 1983 Orbital cobalt irradiation combined with systemic corticosteroids for Graves’ ophthalmopathy: comparison with systemic corticosteroids alone. J Clin Endocrinol Metab 56: 1139-1144.
- Marcocci C, Bartalena L, Bogazzi F, Bruno-Bossio G, Lepri A, Pinchera A 1991 Orbital radiotherapy combined with high-dose systemic glucocorticoids for Graves’ ophthalmopathy is more effective than orbital radiotherapy alone: results of a prospective study. J Endocrinol Invest 14: 853-860.
- Kahaly G, Schrenzemeir, Krause U, Schweikert B, Meuer S, Muller W 1986 Ciclosporin and prednisone v. Prednisone in treatment of Graves’ ophthalmopathy: a controlled, randomized and prospective study. Eur J Clin Invest 16: 415-422.
- Prummel MF, Mourits MP, Berghout A, Krenning EP, van der Gaag R, Koornneef L, Wiersinga AM 1989 Prednisone and cyclosporine in the treatment of severe Graves’ ophthalmopathy. N Engl J Med 321: 1353-1359.
- Bartalena L 2010 What to do for moderate-to-severe Graves’ orbitopathy if glucocorticoids fail? Clin Endocrinol (Oxf) 73: 149-152.
- Salvi M, Vannucchi G, Beck-Peccoz P 2013 Potential utility of rituximab for Graves’ orbitopathy. J Clin Endocrinol Metab 98: 4291-4299.
- Minakaran N, Ezra DG 2013 Rituximab for thyroid-associated ophthalmopathy. Cochrane Database Syst Rev. 2013 May 31;5:CD009226. doi: 10.1002/14651858.
- Stan MN, Garrity JA, Carranza Leon BG, Prabin T, Bradley EA, Bahn RS 2015 Randomized controlled trial of rituximab in patients with Graves’ orbitopathy. J Clin Endocrinol Metab 100: 432-441.
- Salvi M, Vannucchi G, Currò N, Campi I, Covelli D, Dazzi D et al. 2015 Efficacy of B-cell targeted therapy with rituximab in patients with active moderate to severe Graves’ orbitopathy: a randomized controlled study. J Clin Endocrinol Metab 100: 422-431.
- Wiersinga WM 2017 Advances in treatment of active, moderate-to-severe Graves’ ophthalmopathy. Lancet Diabetes Endocrinol 5: 134-142.
- Ye X, Bo X, Hu X, Cui H, Lu B, Shao J, Wang J 2017 Efficacy and safety of mycophenolate mofetil in patients with active moderate-to-severe Graves’ orbitopathy. Clin Endocrinol (Oxf) 86: 247-255.
- Kahaly GJ, Riedl M, Konig J, Pits S, Ponto K, Diana T et al 2018 Mycophenolate plus methylprednisolone versus methylprednisolone alone in active, moderate-to-severe Graves’ orbitopathy (MINGO): a randomized, observer-masked, multicentre trial. Lancet Diabetes Endocrinol, in press.
- Riedl M, Kuhn A, Kramer I, Kolbe E, Kahaly GJ 2016 Prospective, systematically recorded mycophenolate safety data in Graves’ orbitopathy. J Endocrinol Invest 39: 687-694.
- Smith TJ, Huetwell FGL, Hegedus L, Douglas RS 2012 Role of insulin-like growth factor-1 (IGF-1) pathway in the pathogenesis of Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab 26: 291-302.
- Smith TJ, Kahaly GJ, Ezra DG, Fleming JC, Dailey RA, Tang RA et al 2017 Teprotumumab for thyroid-associated ophthalmopathy. N Engl J Med 376: 1748-1761.
- Piantanida E, Bartalena L 2017 Teprotumumab: a new avenue for the management of moderate-to-severe and active Graves’ orbitopathy? J Endocrinol Invest 40: 885-887.
- Baldeschi L 2017 Orbital decompression. In Wiersinga WM, Kahaly GJ (eds), Graves’ orbitopathy. A multidisciplinary approach – Questions and answers, Karger, Basel, 3rd ed., 211-229.
- Mourits MP, Bijl H. Altea MA, Baldeschi L, Boboridis K, Currò N, Dickinson AJ, Eckstein A, Freidel M, Guastella C, Kahaly GJ, Kalmann R, Krassas GE, Lane CM, Lareida J, Marcocci C, Marinò M, Nardi M, Mohr Ch, Neoh C, Pinchera A, Orgiazzi J, Pitz S, Saeed P, Salvi M, Sellari-Franceschini S, Stahl M, von Arx G, Wiersinga WM 2009 Outcome of orbital decompression for disfiguring proptosis in patients with Graves’ orbitopathy using various surgical procedures. Br J Ophthalmol 93: 1518-1523.
- Garrity JA, Fatourechi V, Bartley GB, Bergstrahl EJ, DeSanto LW, Gorman CA 1994 Graves’ ophthalmopathy. Results of transantral orbital decompression in 428 patients with severe Graves’ ophthalmopathy. Am J Ophthalmol 116: 533-547.
- Nardi M, Eckstein A 2017 Eye muscle surgery. In Wiersinga WM, Kahaly GJ (eds), Graves’ orbitopathy. A multidisciplinary approach – Questions and answers, Karger, Basel, 3rd ed., 230-246.
- Clarke L, Eckstein A 2017 Eyelid surgery. In Wiersinga WM, Kahaly GJ (eds), Graves’ orbitopathy. A multidisciplinary approach – Questions and answers, Karger, Basel, 3rd ed., 247-259.
- Marcocci C, Bartalena L, Pinchera A 1998 Ablative or non-ablative therapy for Graves’ hyperthyroidism in patients with ophthalmopathy? J Endocrinol Invest 21: 468-471.
- Weetman AP, Harrison BJ 1998 Ablative or non-ablative therapy for Graves’ hyperthyroidism in patients with ophthalmopathy? J Endocrinol Invest 21: 472-475.
- DeGroot LJ, Benjasuratwong Y 1996 Evaluation of thyroid ablative therapy for ophthalmopathy of Graves’ disease. Orbit 15: 187-196.
- Moleti M, Mattina F, Salomone I, Violi MA, Nucera C, Baldari S, Lo Schiavo MG, Regalbuto C, Trimarchi F, Vermiglio F 2003 Effects of thyroidectomy alone or followed by radioiodine ablation of thyroid remnants on the outcome of Graves’ ophthalmopathy. Thyroid 13: 653-658.
- Menconi F, Marinò M, Pinchera A, Rocchi R, Mazzi B, Nardi M, Bartalena L, Marcocci C 2007 Effects of total thyroid ablation vs near-total thyroidectomy alone on mild to moderate Graves’ orbitopathy treated with intravenous glucocorticoids. J Clin Endocrinol Metab 92: 1653-1658.
- Leo M, Marcocci C, Pinchera A, nardi M, Megna L, Rocchi R, Latrofa F, Altea MA, Mazzi B, Sisti E, Profilo MA, Marinò M 2012 Outcome of Graves’ orbitopathy after total thyroid ablation and glucocorticoid treatment: follow-up of a randomized clinical trial. J Clin Endocrinol Metab 97: E44-E48.
- Elbers L, Mourits M, Wiersinga W 2011 Outcome of very long-term treatment with antithyroid drugs in Graves’ hyperthyroidism associated with Graves’ orbitopathy. Thyroid 21: 279-283.
- Laurberg P, Berman BC, Andersen S, Bulow Pedersen I 2011 Sustained control of Graves’ hyperthyroidism during long-term low-dose antithyroid drug therapy of patients with severe Graves’ orbitopathy. Thyroid 21: 951-956.
- Bartalena L 2011 The dilemma of how to manage Graves’ hyperthyroidism in patients with associated orbitopathy. J Clin Endocrinol Metab 96: 592-599.
- Bartalena L, Macchia PE, Marcocci C, Salvi M, Vermiglio F 2015 Effects of treatment modalities for Graves’ hyperthyroidism on Graves’ orbitopathy: a 2015 Italian Society of Endocrinology consensus statement. J Endocrinol Invest 38: 481-487.
- Moleti M, Sturniolo G, Vermiglio F 2016 Safety of total thyroid ablation in patients with Graves’ orbitopathy. J Endocrinol Invest 39: 1199-1201.
- Fatourechi V 2012 Thyroid dermopathy and acropachy. Best Pract Res Clin Endocrinol Metab 26: 553-565.
- Fatourechi V, Bartley GB, Eghbali-Fatourechi GZ, Powell CC, Ahmed DD, Garrity JA 2003 Graves’ dermopathy and acropachy are markers of severe Graves’ ophthalmopathy. Thyroid 13: 1141-1144.
- Bartley GB, Fatourechi V, Kadrmas EF, Ilstrup DM, Garrity JA, Gorman CA 1996 Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol 121: 284-290.
- Schwartz KM, Fatourechi V, Ahmed DDF, Pond GR 2002 Dermopathy of Graves’ disease (pretibial myxedema): long-term outcome. J Clin Endocrinol Metab 87:438-446.
- Tong DW, Ho KK 1998 Pretibial myxedema presenting as a scar infiltrate. Australas J Dermatol 39:255-257.
- Misner CS, Ramsay EW, Houck He, Kauffman CL 1998 Graves’disease presenting as a localized myxedema in a thigh donor graft site. J Am Ac Dermatol 39:864-869,1998.
- Cohen JB, Balzer B, Wapnir I, McDougall IR 2004 Elephantiasic pretibial myxedema. Thyroid 14: 237-238.
- Fatourechi V 2005 Pretibial myxedema: pathophysiology and treatment options. Am J Clin Dermatol 6: 295-309.
- Shishiba Y, Imai Y, Odajima R, Ozawa Y, Shimizu T 1992 Immunoglobulin G of patients with circumscribed pretibial myxedema of Graves' disease stimulates proteoglycan synthesis in human skin fibroblasts in culture. Acta Endocrinol(Copenh) 127:44-51.
- Hanke CW, Bergfeld WF, Guirguis MN, Lewis LJ 1983 Hyaluronic acid synthesis in fibroblasts of pretibial myxedema. Cleve Clin Q 50:129-133.
- Heufelder AE, Dutton CM, Sarkar G, Donovan KA, Bahn RS 1993 Detection of TSH receptor RNA in cultured fibroblasts from patients with Graves’ ophthalmopathy and pretibial dermopathy. Thyroid 3: 297-300.
- Rapoport B, Alsabeh R, Aftergood D, McLachlan SM 2000 Elephantiasic pretibial myxedema: insight into a hypothesis regarding the pathogenesis of the extrathyroidal manifestations of Graves’ disease. Thyroid 10: 685-692.
- Metcalfe RA, Davies R, Weetman AP 1993 Analysis of fibroblast-stimulating activity in IgG from patients with Graves’ dermopathy. Thyroid 3: 207-212.
- Kahaly GJ, Dillmann WH 2005 Thyroid hormone action in the heart. Endocr Rev 26: 704-728.
- Danzi S, Klein I 2012 Thyroid hormone and the cardiovascular system. Med Clin N Am 96: 257-268.
- Kahaly GJ, Wagner S, Nieswandt J, Mohr-Kahaly S, Rayan TJ 1999 Stress echocardiography in hyperthyroidism. J Clin Endocrinol Metab 84:2308-2313.
- Franklyn JA, Maisonneuve P, Sheppard MC, Betteridge J, Boyle P 1998 Mortality after the treatment of hyperthyroidism with radioactive iodine. N Engl J Med 338: 712-718.
- Osman F, Gammage MD, Franklyn JA 2002 Hyperthyroidism and cardiovascular morbidity and mortality. Thyroid 12: 483-488.
- Parle JV, Maisonneuve P, Sheppard MC, Boyle P, Franklyn JA 2001 Prediction of all cause and cardiovascular mortality in elderly people from one low serum thyrotropin result : a 10-year cohort study. Lancet 358: 861-865.
- Kahaly GJ, Nieswandt J, Mohr-Kahaly S 1998 Cardiac risk of hyperthyroidism in the elderly. Thyroid 8:1165-1169.
- Agner T, Almdal T, Thorsteinsson B, Agner E 1984 A reevaluation of atrial fibrillation in thyrotoxicosis. Dan Med Bull 31: 157-159.
- Nakazawa HK, Sakurai K, Hamada N, Momotani N, Ito K 1982 Management of atrial fibrillation in the post-thyrotoxic state. Am J Med 72:903-906.
- Sawin LT, Geller A, Wolf PhA, Belanger A, Baker E 1994 Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. New Engl J Med 331:1249-1253.
- Biondi B 2012 Heart failure and thyroid dysfunction. Eur J Endocrinol 167: 609-618.
- Siu CW, Yeung CY, Lau CP, Kung AW, TSE HF 2007 Incidence, clinical characteristics and outcome of congestive heart failure as the initial presentation in patients with primary hyperthyroidism. Heart 93: 483-487.
- Yue W-S, Chong B-H, Zhang X-H, Liao S-Y, Jim A-Y, Jim M-H, Kung AWC, Tse H-F, Siu C-W 2011 Hyperthyroidism-induced left ventricular diastolic dysfunction: implication in hyperthyroidism-related heart failure. Clin Endocrinol (Oxf) 74: 636-643.
- Boccalandro C, Boccalandro F, Orlander P, Wei CF 2003 Severe reversible dilated cardiomyopathy and hyperthyroidism: case report and review of the literature. Endocr Pract 9:140-6.
- Soh MC, Croxson M 2008 Fatala thyrotoxic cardiomyopathy in a young man. Br Med J 337: a531.
- Featherstone HJ, Stewart DK 1983 Angina in thyrotoxicosis: thyroid related coronary artery spasm. Arch Intern Med 143: 554-558.
- Moliterno D, Debold CR, Robertson RM 1992 Coronary vasospasm – relation to the hyperthyroid state. Am J Med Sci 304: 38-42
- Resenkov L, Falicov R 1977 Thyrotoxicosis and lactate producing angina pectoris with normal coronary arteries. Br Heart J 39:1051-1055
- Biondi B, Fazio S, Carella C, Amato G, Littadini A, Lupoli G, Saca L, Bellastella A, Lombardi G. 1993 Cardiac effects of long-term thyrotropin-suppressive therapy with levothyroxine. J Clin Endocrinol Metab 77:334-338.
- Shapiro LE, Sievart R, Ong L, Ocamo E, Chance R, Lee M, Nanna M, Ferrick K, Surks M 1997 Minimal cardiac effects in asymptomatic athyreotic patients chronically treated with thyrotropin-suppressive doses of L-thyroxine. J Clin Endocrinol Metab 82:2592-2595.
- Nakazawa H, Lythall DA, Noh J, Ishikawa N, Sugino K, Ito K, Hardman SM 2000 Is there a place for late cardioversion of atrial fibrillation? A long-term follow-up study of patients with post-thyrotoxic atrial fibrillation. Eur Heart J 12:327-333.
- The 2021 European Group on Graves' orbitopathy (EUGOGO) clinical practice guidelines for the medical management of Graves' orbitopathy.[Eur J Endocrinol. 2021]The 2021 European Group on Graves' orbitopathy (EUGOGO) clinical practice guidelines for the medical management of Graves' orbitopathy.Bartalena L, Kahaly GJ, Baldeschi L, Dayan CM, Eckstein A, Marcocci C, Marinò M, Vaidya B, Wiersinga WM, EUGOGO †. Eur J Endocrinol. 2021 Aug 27; 185(4):G43-G67. Epub 2021 Aug 27.
- Review Current concepts regarding Graves' orbitopathy.[J Intern Med. 2022]Review Current concepts regarding Graves' orbitopathy.Bartalena L, Tanda ML. J Intern Med. 2022 Nov; 292(5):692-716. Epub 2022 Jun 1.
- Review Extrathyroidal manifestations of Graves' disease: a 2014 update.[J Endocrinol Invest. 2014]Review Extrathyroidal manifestations of Graves' disease: a 2014 update.Bartalena L, Fatourechi V. J Endocrinol Invest. 2014 Aug; 37(8):691-700. Epub 2014 Jun 10.
- The 2016 European Thyroid Association/European Group on Graves' Orbitopathy Guidelines for the Management of Graves' Orbitopathy.[Eur Thyroid J. 2016]The 2016 European Thyroid Association/European Group on Graves' Orbitopathy Guidelines for the Management of Graves' Orbitopathy.Bartalena L, Baldeschi L, Boboridis K, Eckstein A, Kahaly GJ, Marcocci C, Perros P, Salvi M, Wiersinga WM, European Group on Graves' Orbitopathy (EUGOGO). Eur Thyroid J. 2016 Mar; 5(1):9-26. Epub 2016 Mar 2.
- Review Graves' orbitopathy: imperfect treatments for a rare disease.[Eur Thyroid J. 2013]Review Graves' orbitopathy: imperfect treatments for a rare disease.Bartalena L. Eur Thyroid J. 2013 Dec; 2(4):259-69. Epub 2013 Nov 20.
- Graves’ Disease: Complications - EndotextGraves’ Disease: Complications - Endotext
Your browsing activity is empty.
Activity recording is turned off.
See more...
